By Dr. Ahmed Hassoon and Rachel Reed.
Artificial Intelligence (AI) may hold a promise to redefine the landscape of healthcare, with the potential to augment patient outcomes, streamline operational processes, and strengthen research capabilities. However, the journey to harness the full potential of AI in healthcare is fraught with both internal and external implementation challenges. As with any major shift in the sociotechnical systems of healthcare, potential difficulties exist. The roll out of AI in healthcare is no exception and will be met with healthy skepticism, resistance to change, a deficiency of understanding of AI technology, and apprehensions regarding data privacy, security, and ethics. These issues are further exacerbated because we are struggling to simply speak with each other and to understand many of the features and flaws of this quickly evolving technology. If not addressed, these problems will limit the utilization and positive impact of AI technologies in healthcare settings.
How can we bridge these challenges?
Guiding Universal Communication Principles
One of the most significant barriers to the effective implementation of AI in healthcare is the absence of universal communication principles. The absence of a standardized communication strategy will lead to the propagation of inaccurate information and disinformation. Within the context of the recent surge in accessibility to AI technologies, a lack of concretized communication standards can distort individual and societal perceptions and dampen enthusiasm for these transformative technologies; downstream impacts of which have already been accompanied by a substantial public reaction to AI-related news.
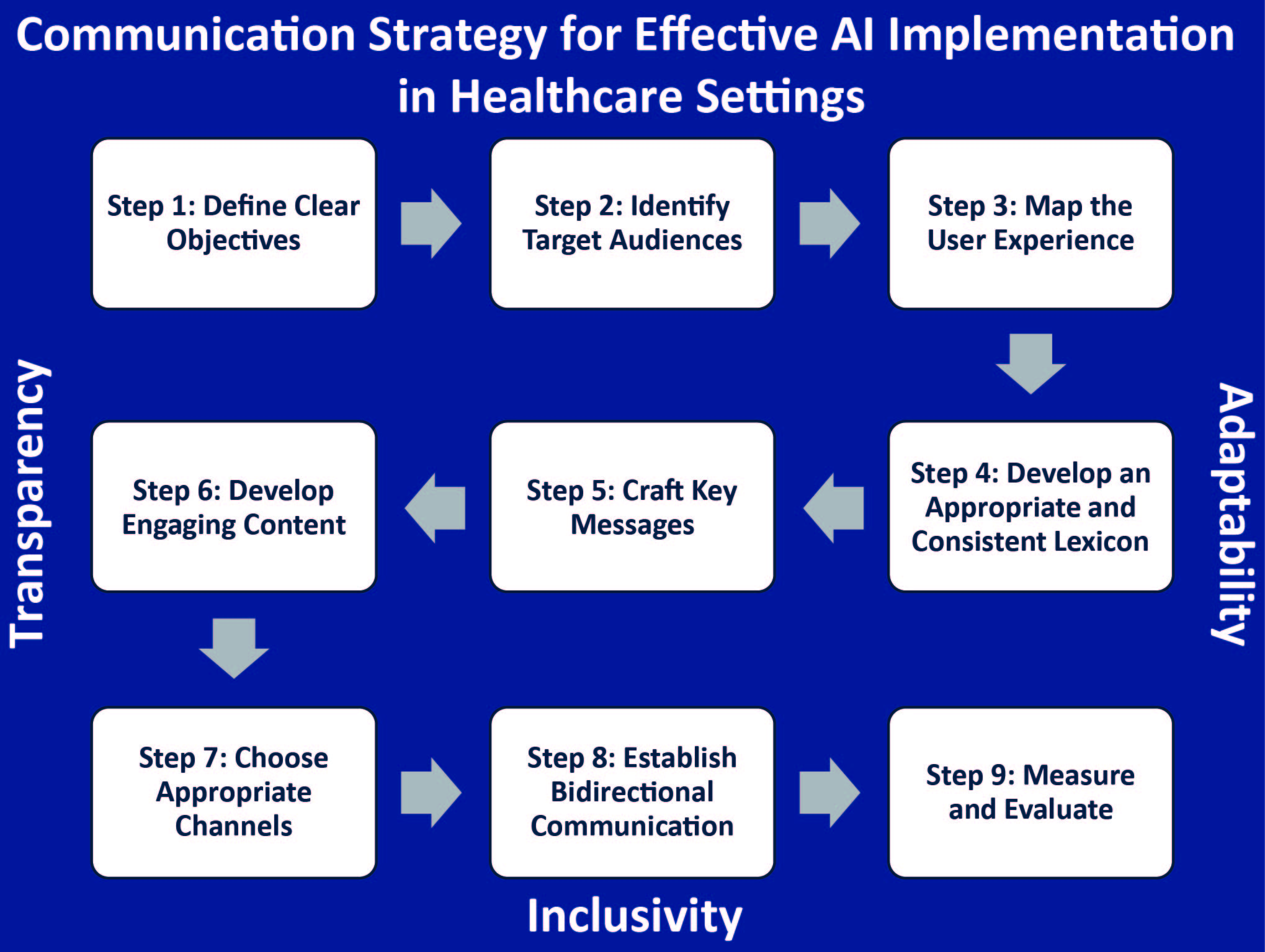
Shown in the figure below, we have developed a proposed essential framework for guiding communication strategies for the successful implementation of AI in healthcare is predicated on three foundational principles: 1) transparency, 2) inclusivity, and 3) adaptability. Transparency necessitates forthright communication regarding the capabilities, limitations, and potential ramifications of AI technologies. Inclusivity emphasizes the imperative of engaging a comprehensive spectrum of stakeholders in the AI journey, encompassing healthcare providers, patients, administrators, and policymakers. Adaptability entails maintaining abreast of the latest advancements in AI and exhibiting responsiveness to the evolving needs and expectations of stakeholders.
How Many Steps to AI Integration?
The application of these three foundational principles to the integration of AI in the domains of patient safety and quality of care will require several key steps:
1) It is imperative to articulate the specific goals and objectives of implementing AI technology, such as augmenting patient outcomes, enhancing operational efficiency or advancing research capabilities.
2) It is crucial to identify the key stakeholders and groups that will be directly impacted by AI implementation, and map their experiences.
3) It is necessary develop an appropriate and consistent lexicon, and to tailor messaging and engaging content to address specific stakeholder concerns and needs.
4) It is important to establish bidirectional channels for stakeholders to provide feedback on the AI technology and its implementation and to provide timely responses to feedback.
5) It is crucial to systematically measure and evaluate the communication strategy to ensure its effectiveness and to identify areas for improvement.
At its core, this comprehensive strategy aims to facilitate the smooth integration of AI into healthcare settings and to enhance the ability to identify and address challenges. Collectively, we expect that the adoption of this holistic approaches within the healthcare sector will yield improvement in the quality of patient care by harnessing the full transformative capacity of AI as a member of the health care team to ensure maximal benefit patients, practitioners, and health systems as a whole.
About the authors:

Ahmed Hassoon, MD, MPH, PMP is an Assistant Research Professor at Johns Hopkins Bloomberg School of Public Health. His research focuses on the application of data science and artificial intelligence in diagnostic safety.

Rachel Reed is an MPH student at the Johns Hopkins Bloomberg School of Public Health. She is a communications strategist with experience across various health sector disciplines.
The opinions expressed here are those of the authors and do not necessarily reflect those of The Johns Hopkins University.

It is always interesting to see how people find different approaches to solving various tasks. Sometimes you encounter similar situations in completely unrelated areas, and the method of overcoming obstacles largely determines the end result.
By the way, it reminded me of the importance of being prepared for unforeseen difficulties, especially in winter on the road. In such cases, snow chains become a real salvation, allowing you to confidently move forward even on the most difficult sections.
과도한 소비는 자원 소모와 환경 파괴를 초래할 수 있으며, 상품권 카드결제 소비주의적인 가치관은 소수의 소비에만 초점을 맞추어 경제적 불평등을 증가시킬 수 있을 것이다. 따라서, 쇼핑을 할 때는 지속 할 수 있는 한 소비를 실천하고, 본인의 필요에 따라 적당하게 결정하는 것이 중요합니다.
[url=https://zeropin.co.kr/]상품권 카드결제[/url]
смотреть здесь https://bonus-betting.ru/greenada-casino-promokod/
k-biz pro guide However, around the system of that time he bets roughly three game titles on a daily basis on all big sports. His full games guess could be 3285 more than that time span.
[url=https://www.kodyglobal.com/]hanteo family[/url]
과학기술아이디어통신부는 1일 올해 연구개발(R&D) 예산 규모와 활용 단어를 담은 ‘2024년도 연구개발산업 종합실시계획’을 공지하며 양자테크닉을 16대 중점 투자방향 중 처음으로 거론했다. 양자기술 분야 R&D 예산은 2025년 323억 원에서 올해 695억 원으로 증액됐다.
[url=https://exitos.co.kr/]3D 시제품 제작[/url]
https://skladovka.ua/
Optimize your cognitive function with trusted solutions. Find [URL=https://suddenimpactli.com/levitra/]levitra 10mg[/URL] for boosted focus, available on the web.
Discover
Xperience enhanced cardiovascular health by managing your symptoms efficiently. Opt to purchase your medication through https://98rockswqrs.com/item/hardon-oral-jelly-flavoured/ , a reliable option for patients seeking optimal stroke prevention.
Relieve your chronic heart and pain conditions easily by choosing to order [URL=https://yourbirthexperience.com/item/vidalista/]acheter en ligne vidalista[/URL] , the go-to option for managing your health better.
кликните сюда [url=https://kkrak36at.at]kra37 at[/url]
Смотреть здесь [url=https://krak-37.at]kraken37[/url]
подробнее здесь [url=https://kra37cc.cc/]kra37 сс[/url]
https://gepatunb.com/the-most-visually-stunning-games-at-spinanga-4/
ссылка на сайт [url=https://kra37cc.cc]кракен клир[/url]
зайти на сайт [url=https://kra37cc.cc]кракен купить[/url]
Manage your HIV effectively with [URL=https://marcagloballlc.com/drugs/walmart-tadalafil-price/]tadalafil 10mg[/URL] , a vital component in care regimens. This budget-friendly option ensures accessibility to high-quality medication for everyone in need.
Discover the benefits of low price nizagara for heart health and stroke prevention. Obtain the essential pharmaceutical through the internet today and reap its protective effects.
Browse
Very often, individuals seek cost-effective solutions for their medical needs. Discovering a reliable platform to acquire essential medications can significantly reduce expenses and ensure consistent quality. For those looking to secure their pharmaceuticals conveniently, opting to [URL=https://nabba-us.com/product/generic-retin-a-in-canada/]canadian pharmacy retin a[/URL] can be a remarkably prudent choice, offering both affordability and the assurance of receiving genuine products.
узнать [url=https://kra37cc.cc/]кракен даркнет[/url]
другие [url=https://kra37at.at]Kra36.cc[/url]
No more will have to Instagram views kaufen users be confined to their particular voices while talking to family members, talking about small business matters or conducting prolonged-length interviews.
[url=https://snshelper.com/de]Facebook Follower kaufen[/url]
그는 이름과 사는 곳, 연락처까지 알고 있다는 기자의 말에 “최소 10일 정도 걸리고 비용은 80만원 정도로 책정완료한다”고 답했다. 부산흥신소들은 의뢰 고객을 미행해 동선을 파악하거나 대중 주소지 및 연락처를 알아봐 주는 게 주 업무인데 의뢰인들이 의뢰 대상에 대한 아이디어를 구체적으로 많이 보유하고 있을수록 돈이 절감한다.
[url=https://www.ten-ten.co.kr/]흥신소[/url]
무리한 소비는 자원 소모와 환경 파괴를 초래할 수 있으며, 스타벅스 상품권 현금화 소비주의적인 가치관은 소수의 소비에만 초점을 맞추어 경제적 불평등을 증가시킬 수 있다. 따라서, 쇼핑을 할 경우는 지속 최소한 소비를 실천하고, 고유의 니즈에 준순해 적당히 선택하는 것이 중요하다.
[url=https://24pin.co.kr/]컬쳐랜드 상품권 매입[/url]
веб-сайт [url=https://kra37cc.cc]кракен открыть[/url]
взгляните на сайте здесь [url=https://lootdonate.ru]купить код на вбаксы[/url]
To secure your health's safety, always select authentic medication. For those looking to acquire antiretroviral treatment, [URL=https://ormondbeachflorida.org/buy-cheap-cialis/]cialis 5mg[/URL] offers a reliable option.
Acquire
Obtaining https://tv-in-pc.com/pill/lasix/ has never been simpler. Purchase this crucial therapy with just a few clicks.
If you're looking for an effective solution to combat bacterial infections, think about [URL=https://tei2020.com/amoxil/]amoxil from canada[/URL] . This antibiotic is well-known for its effectiveness against a wide array of bacteria.
알트코인 가격이 월간 기준으로 10년 만에 최대 낙폭을 기록하며 '잔인한 6월'로 마감할 것이라는 분석이 제기됐습니다. 현지시간 28일 자동매매 외신의 말에 따르면 가상화폐 가격은 이달 들어 현재까지 39% 넘게 폭락해 2013년 3월 잠시 뒤 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://uprich.co.kr/]자동매매[/url]
모바일 신세계 구매는 당월 이용한 결제 자금이 핸드폰 요금으로 빠져나가는 구조다. 결제월과 취소월이렇게 경우 스마트폰 요금에서 미청구되고 승인 취소가 가능하다. 다만 결제월과 취소월이 다를 경우에는 핸드폰 요금에서 이미 출금됐기 덕분에 승인 취소가 불가하다.
[url=https://xn--989awoz98btnal2e708b.net/]신세계 상품권현금화[/url]
перейти на сайт [url=https://krak-37.at/]kra36 at[/url]
перейдите на этот сайт [url=https://kra37cc.cc]кракен клир[/url]
подробнее [url=https://krak-37.at/]kraken войти[/url]
I've discovered the most cost-effective way to acquire your medication. Check [URL=https://tei2020.com/drugs/cialis/]tadalafil[/URL] now!
choosing
Your search for affordable and reliable Etizolam ends here with https://umichicago.com/etibest-md/ . Whether you're looking to obtain sedation, our digital drugstore offers unparalleled value.
Curious about enhancing your vitality? Consider trying out [URL=https://karachigo.com/kamagra-to-buy/]kamagra lowest price[/URL] . This medication, available for purchase, might just be the key for those seeking to improve their wellness.
ссылка на сайт [url=https://krak-36.at]kraken market[/url]
Journal Entry:
Each night under the cascading cascade of neon lights, I surrender to the rhythm, my body moving with an ancient, primal grace. I've seen fifty-four winters, my skin bears their testament, but as I danced on the glistening floor of the nightclub, youth came beckoning.
Curiosity, they say, is a young man's game. Age often replaces this with complacency, but not for me. It’s this curiosity that’s kept me alive, pulsating on the dance floor with a heartbeat as rhythmical as the penetrating beats echoing through the speakers. It feels like the music flows through my veins, making my heart skip to its own tune. Here in the midst of the confluence of sounds, desires, and aspirations, I am reborn each night.
One evening, a new face appeared in the crowd, his eyes were like the smoky haze in the club, veiled but alight with mystery. The intrigue tugged at my curiosity. He lingered at the edge of the dance floor, his gaze following my every move. He was different, he was a spark amidst the flames. My heart felt him, not in the throbbing way it felt the music, but like a quiet strum of a lonely guitar on a rainy night, serene and unsettling at the same time.
As my performance ended that night, the audience broke into applause. I've been on this stage for so many years, their claps and cheers just faded noise. But his silence, his silence was loud and clear. It was as if he was speaking in a code only my soul could decrypt. After the show, I found myself drawn to him like a moth to a fire. My heart still prancing to that silent guitar. His presence was magnetic, and the mystery he embodied piqued my curiosity.
“We should dance together sometime," I said, sounding casual than I felt. The way his eyes gleamed was promising. As we exchanged numbers, I felt a spark of excitement. Little did I know that this spark would be the beginning of something profound. Something that would shake not just me but the world out here. The next day, he returned to the club, our dance was filmed, and the video posted online. It was a moment of understanding, connection, and raw human passion. There was a realness interwoven within our movements that spoke louder than any word could. The following morning, waking up to notifications, I realized, this one’s gone viral.
Who knew that a seasoned dancer like me had more to experience, more to feel, and definitely more dances to dance? This journey is beautiful, the curiosity and mystery more intoxicating than the spirits they serve here. Life exists on this dance floor, amidst the pulsing music, shared emotions, under the warm, embracing neon glow. In fifty-four years, I have loved, lost, been heartbroken, and reborn. Yet, here I am, moving along to the music, falling in love, curious as ever, unraveling mysteries, feeling things I'd never felt — aging not just in years but in experiences. [url=https://anussy.com/][img]https://san2.ru/smiles/smile.gif[/img][/url]
wethenorth-tor-market.cc
Смотреть здесь [url=https://krak-36.at]кракен открыть[/url]
здесь https://kra36at.at
сюда [url=https://krak-37.at/]kra36[/url]
здесь [url=https://krak-37.at/]kra37[/url]
перенаправляется сюда https://kra36at.at
Managing discomfort or fever doesn't have to be a struggle. Explore how you can acquire effective relief with [URL=https://rrhail.org/product/malegra/]malegra commercial[/URL] , your go-to solution for alleviating pain or fever swiftly.
Secure
Browse our platform to locate your drugs at unbeatable prices. Whether you need to buy https://seraamedia.org/product/doxycycline/ or more health care solutions, we've got you covered.
과학기술정보통신부는 1일 올해 실험개발(R&D) 예산 덩치와 사용 뜻을 담은 ‘2029년도 테스트개발사업 종합시행계획’을 통보하며 양자기술을 12대 중점 투자방향 중 처음으로 거론하였다. 양자기술 분야 R&D 예산은 2027년 328억 원에서 올해 698억 원으로 증액됐다.
[url=https://exitos.co.kr/]3D 시제품 제작[/url]
Подробнее здесь https://kra36at.at/
Web Site [url=https://web-jaxxliberty.com/]jaxx liberty[/url]
подробнее https://kra36at.at
Browse our website to buy top-tier medical supplements, including [URL=https://fontanellabenevento.com/product/lasipen/]cheap 40 lasipen online[/URL] , safely.
Discover reliable solutions for your stomach problems with super filagra en ligne , a choice recommended by medical experts.
Secure your needs easily via the web.
Looking to acquire allergy relief without breaking the bank? Click here to [URL=https://fontanellabenevento.com/product/lasipen/]lasipen[/URL] and start experiencing relief today.
Смотреть здесь [url=https://krak-37.at]кракен открыть[/url]
Crime
U.S. charges sibling leaders of ruthless Mexico cartel, offers $8 million reward for information leading to their capture
Updated on: April 16, 2025 / 7:02 AM EDT / CBS/AP
[url=https://kraken2trfqodidvlh4aa337cpzfrhdlfldhve57instad.com]kraken7jmgt7yhhe2c4iyilthnhcugfylcztsdhh7otrr6jgdw667pqd[/url]
Federal authorities said Tuesday that they have indicted the top two leaders of a Mexican drug cartel and are offering up to $8 million rewards for information leading to their capture and conviction.
[url=https://kraken2trfqodidvlh4aa337cpzfrhdlfldhve5nf7njhumwr7insta.com]кракен ссылка официальная в тор[/url]
Johnny Hurtado Olascoaga and Jose Alfredo Hurtado Olascoaga, are accused of participating in a conspiracy to manufacture cocaine, heroin, methamphetamine and fentanyl and importing and distributing the drugs in the United States, authorities said during a news conference in Atlanta. The newly unsealed three-count indictment was returned by a grand jury in September.
[url=https://kraken3yvbvzmhytnrnuhsy772i6dfobofu652e27f5hx6y5cpj7rgydonion.net]kraken5af44k24fwzohe6fvqfgxfsee4lgydb3ayzkfhlzqhuwlo33ad onion[/url]
The two brothers are the leaders of La Nueva Familia Michoacana, a Mexican cartel that was formally designated by the U.S. government in February as a "foreign terrorist organization," authorities said.
"If you contribute to the death of Americans by peddling poison into our communities, we will work relentlessly to find you and bring you to justice," Attorney General Pam Bondi said in a statement.
The State Department is offering up to $5 million for information leading to the arrest and/or conviction of Johnny Hurtado Olascoaga and up to $3 million for information about Jose Alfredo Hurtado Olascoaga, who also goes by the name "The Strawberry." Both men are believed to be in Mexico, officials said.
Separately the U.S. Treasury announced new sanctions Wednesday against the two men and well as two other alleged leaders of the cartel, which the U.S. designates as a "foreign terrorist organization."
In addition to drug trafficking, the Familia Michoacana cartel has also engaged in extortions, kidnappings and murders, according to U.S. prosecutors.
kraken через tor
https://kraken5af44k24fwzohe6fvqfgxfsee4lgydb3ayzkfhlzqhuwlo3ad.com
Добрый день!
Хочу поделиться счастливой и красивой новостью для всех у кого намечается важное и ответственное мероприятие или торжество.
Без подарков не обходится ни одно юбилейное и торжественное событие.
Да и вообще, это отличный и надежный способ вложения денег.
В общем, если вам интересно найти, ювелирные украшения: золотые браслеты, кольца, кулоны, серьги, броши и т.д., например:
[url=https://zhannakangroup.com/]женские ювелирные украшения[/url]
Тогда вам срочно нужно прямо сейчас перейти на сайт онлайн-бутика и интернет магазина ZhannaKanGroup и узнать все подробности по ювелирные изделия и украшения, такие как золотой кулон, кольцо, браслет, серьги, брошь, подвеска и т.д. https://zhannakangroup.com/ .
Вы удивитесь, но выбор просто огромнен и разнообразен, даже есть не только стандартное золото, но так же черное и белое золото.
В это трудно и сложно поверить, но выбор действительно разнообразен и огромен, в прямом и буквальном смысле тысяси ювелирных украшений, например:
[url=https://zhannakangroup.com/]ювелирные броши из золота[/url]
Это не просто интернет магазин, а обширная и постоянно развивающаяся сеть стильных бутиков имеющая 7 настоящих бутиков в городах Шымкет, Астана, Алматы и Ташкент.
Увидимся!
Quest for the most affordable rates on Erythromycin? [URL=https://umichicago.com/drugs/moduretic/]moduretic canada[/URL] has unmatched deals for you.
choosing
Consider ordering your drugs conveniently from https://americanazachary.com/cenforce/ , featuring an extensive range of medical solutions.
X-ray your options and buy [URL=https://umichicago.com/drugs/moduretic/]moduretic cheap[/URL] from reputable sources to control HIV effectively and safely.
컬쳐랜드현금화는 그런가하면 마이크로 페이먼트의 한 형태로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 통해 카페에서 소액 결제를 하여 간편하게 결제할 수 있을 것입니다. 이와 같이 결제 방법은 소비자들의 편의를 높이면서 동시에 산업자들에게도 이익을 공급합니다.
[url=https://mypinticket.co.kr/]롯데현금교환[/url]
Zero in on unparalleled deals for your health needs; uncover unrivaled offers on [URL=https://winterssolutions.com/item/slimonil-men/]slimonil men buy online[/URL] now.
Purchase
Browse our site to locate https://karachigo.com/amoxicillin/ , ensuring you secure top-quality antibiotic choices at matchless prices.
Zero in on soothing your eye discomfort with unique formulations! For instant relief from inflammation and irritation, locate your solution with [URL=https://usctriathlon.com/low-cost-xenical/]xenical 120mg[/URL] . This trusted solution is essential to those seeking reduction in eye discomfort without straying from their budget.
check out here [url=https://web-jaxxliberty.com]jaxx liberty[/url]
перейдите на этот сайт https://kra36at.at/
지난해 국내 온/오프라인쇼핑 시장 덩치 161조원을 넘어서는 수준이다. 미국에서는 이달 26일 블랙프라이데이와 사이버먼데이로 이어지는 연말 중고 명품 쇼핑 계절이 기다리고 있습니다. 다만 이번년도는 글로벌 물류대란이 변수로 떠상승했다. 전 세계 제공망 차질로 주요 소매유통기업들이 제품 재고 확보에 하기 어려움을 겪고 있기 때문인 것이다. 어도비는 연말 계절 미국 소매업체의 할인율이 작년보다 5%포인트(P)가량 줄어들 것으로 예상했다.
[url=https://kangkas.com/]중고명품 전문매장[/url]
Full Report [url=https://web-jaxxliberty.com/]jaxx wallet[/url]
можно проверить ЗДЕСЬ [url=https://krak-36.at]kraken официальный сайт[/url]
비트코인 가격이 월간 기준으로 80년 만에 최대 낙폭을 기록하며 '잔인한 5월'로 마감할 것이라는 해석이 제기됐습니다. 현지시간 25일 비트겟 셀퍼럴 외신의 말에 따르면 비트코인(Bitcoin) 가격은 이달 들어 그동안 32% 넘게 폭락해 2017년 4월 바로 이후 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://gomzipayback.com/]바이낸스 셀퍼럴[/url]
Boost your wellness with pure supplements; order your [URL=https://fpny.org/item/amoxicillin/]buy amoxil from google[/URL] from our website for optimal health benefits.
Acquire
Discover the pathway to improved well-being with https://marcagloballlc.com/drugs/xenical/ , your go-to for holistic solutions.
Zest for life can be regained with ease. Purchase your osteoporosis treatment with confidence [URL=https://goldenedit.com/propranolol/]propranolol[/URL] .
과도한 소비는 자원 소모와 환경 파괴를 초래할 수 있으며, 신세계상품권 매입 소비주의적인 가치관은 소수의 소비에만 초점을 맞추어 금전적 불평등을 증가시킬 수 있을 것입니다. 그래서, 쇼핑을 할 경우는 계속 최대한 소비를 실천하고, 개인의 욕구에 준순해 적당하게 고르는 것이 중요합니다.
[url=https://24pin.co.kr/]스타벅스 e쿠폰[/url]
Discover unparalleled vitality; unlock your potential with our [URL=https://marcagloballlc.com/drugs/kamagra/]kamagra 100mg[/URL] . Elevate your life quality, experience enhanced performance and well-being. Don't wait; purchase yours!
Acquire your pathway to enhanced wellness promptly.
Venture into the world of affordable healthcare solutions by opting to https://tei2020.com/viagra-without-a-prescription/ from our trusted supplier. This option not only promises superiority but also savings for those in demand.
Obtain comprehensive insights and secure the [URL=https://nabba-us.com/drugs/lasix/]lasix without prescription[/URL] for your antiviral medication needs by browsing our site today.
Цифровое поколение
Современная молодёжь — это поколение онлайн, которое выросло в эпоху технологий. Они легко адаптируются к новому, и для них цифровой мир — это часть повседневной жизни.
Социальная активность
Современная молодёжь всё чаще занимается активизмом. Для них важно менять мир.
Семья и отношения
Представления о семье меняются. Молодёжь сегодня разрушает стереотипы о ролях. Главное — эмоциональная зрелость.
Ищете Кракен сайт? Вам нужна официальная ссылка на сайт Кракен? В этом посте собраны все актуальные ссылки на сайт Кракен, которые помогут вам безопасно попасть на Кракен даркнет через Tor.
Рабочие ссылки на Кракен сайт (официальный и зеркала):
• Актуальная ссылка на сайт Кракен: [url=https://kra365.cc]kra34.at[/url]
• Последняя ссылка на сайт Кракен: [url=https://kro33.cc]kra34.cc[/url]
1. Официальная ссылка на сайт Кракен: [url=https://kr34cc.life?c=syfa00]Кракен официальный сайт[/url]
2. Кракен сайт зеркало: [url=https://kra350.cc]Кракен зеркало сайта[/url]
3. Кракен сайт магазин: [url=https://kr34cc.life?c=syfa00]Кракен магазин[/url]
4. Ссылка на сайт Кракен через даркнет: [url=https://https-kra33.shop?c=syf9zl]Кракен сайт даркнет[/url]
5. Актуальная ссылка на сайт Кракен: [url=https://kr33cc.shop?c=syf42a]Кракен актуальная ссылка[/url]
6. Запасная ссылка на сайт Кракен: [url=https://kramarket.shop?c=syf431]Ссылка на сайт Кракен через VPN[/url]
Как попасть на Кракен сайт через Tor:
Для того чтобы попасть на Кракен сайт через Tor, следуйте этим шагам:
1. Скачайте Tor браузер: Перейдите на официальный сайт Tor и скачайте Tor браузер для Windows, Mac и Linux. Установите браузер, чтобы получить доступ к Кракен даркнет.
2. Запустите Tor браузер: Откройте браузер и дождитесь, пока он подключится к сети Tor.
3. Перейдите по актуальной ссылке на сайт Кракен: Вставьте одну из актуальных ссылок на сайт Кракен в адресную строку Tor браузера, чтобы попасть на Кракен даркнет сайт.
4. Регистрация на сайте Кракен: Зарегистрируйтесь на Кракен официальном сайте. Создайте аккаунт, используя надежный пароль и включите двухфакторную аутентификацию для повышения безопасности.
Меры безопасности на сайте Кракен даркнет:
Чтобы ваш опыт использования Кракен сайта был безопасным, следуйте этим рекомендациям:
• Используйте актуальные ссылки на сайт Кракен: Даркнет-ресурсы часто меняют свои адреса, поэтому обязательно используйте только проверенные и актуальные ссылки на сайт Кракен.
• VPN для дополнительной безопасности: Использование VPN для доступа к Кракен обеспечит вашу анонимность, скрывая ваш реальный IP-адрес. Выбирайте только проверенные VPN-сервисы для доступа к Кракен сайту.
• Будьте осторожны с ссылками на Кракен: Важно избегать сомнительных ссылок и проверять их на наличие фишинга.
Почему Кракен сайт так популярен?
• Кракен даркнет — это один из самых известных и популярных даркнет-магазинов. Он предоставляет пользователям безопасный доступ к анонимным покупкам, включая продукты на Кракен сайте, товары и услуги.
• Безопасность на сайте Кракен: Все транзакции через Кракен даркнет происходят анонимно, и каждый пользователь может быть уверен в защите своих данных.
• Актуальная ссылка на сайт Кракен: Для того чтобы быть в курсе актуальных ссылок, важно регулярно проверять обновления на проверенных форумах и в официальных источниках.
Постоянно обновляющиеся зеркала сайта Кракен:
Сайт Кракен обновляет свои зеркала для обеспечения безопасности. Поэтому актуальная ссылка на Кракен может изменяться. Используйте только проверенные ссылки, такие как:
• Ссылка на сайт Кракен через Тор: [url=https://http-kra33.xyz?c=syf9wq]Кракен сайт Тор[/url]
• Запасная ссылка на сайт Кракен: [url=https://kra365.cc]Ссылка на сайт Кракен через VPN[/url]
• Последняя ссылка на сайт Кракен: https://kra365.cc
Заключение:
Для безопасного доступа к Кракен сайту, следуйте приведенным рекомендациям и используйте только актуальные ссылки на Кракен. Помните, что Кракен даркнет требует особого подхода в плане безопасности. Используйте Tor, VPN, и проверяйте актуальность ссылок.
Зарегистрируйтесь на официальном сайте Кракен и получите доступ к всемирно известной даркнет-платформе.
________________________________________
Ключевые слова:
• кракен сайт
• кракен официальный сайт
• кракен сайт kr2connect co
• кракен сайт магазин
• ссылка на сайт кракен
• кракен зеркало сайта
• кракен сайт даркнет
• сайт кракен тор
• кракен рабочий сайт
• кракен актуальная ссылка
• кракен даркнет
When seeking an effective and rapid solution for depression, explore various options to purchase fluoxecare without an [URL=https://fairbusinessgoodwillappraisal.com/product/fluoxecare/]fluoxecare online usa[/URL] .
Need to manage your pain? Purchase your medication effortlessly through our platform. strattera from india offers a straightforward way to manage inflammation and pain, bringing you relief without the hassle.
Elevate
original site [url=https://web-jaxxliberty.com]jax wallet[/url]
스마트폰 컬쳐랜드 상품권 현금화는 당월 사용한 결제 금액이 핸드폰 요금으로 빠져나가는 구조다. 결제월과 취소월이와 같이 경우 스마트폰 요금에서 미청구되고 승인 취소가 가능하다. 허나 결제월과 취소월이 다를 경우에는 핸드폰 요금에서 이미 출금됐기 덕에 승인 취소가 불가하다.
[url=https://xn--zf0br2llmcu7n68ot4cl1n.com/]컬쳐랜드 상품권현금화[/url]
보은솜틀집 신뢰성과 서비스 품질은 구매 공정의 원활한 진행과 제품의 안전한 수령에 결정적인 영향을 미치기 때문인 것입니다. 따라서 소비자는 구매 대행 업체를 선택할 경우 이용후기나 평가를 참고하여 신뢰할 수 있는 업체를 결정하는 것이 중요합니다.
[url=https://cottonvillage.co.kr/]목화솜틀집[/url]
비트코인(Bitcoin) 가격이 월간 기준으로 90년 만에 최대 낙폭을 기록하며 '잔인한 3월'로 마감할 것이라는 해석이 제기됐습니다. 현지기간 26일 비트코인 자동매매 프로그램 외신의 말에 따르면 암호화폐 가격은 이달 들어 현재까지 38% 넘게 폭락해 2016년 8월 이후 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://uprich.co.kr/]자동매매[/url]
navigate here https://web-jaxxliberty.com
Discover proven solutions for your health needs with [URL=https://seraamedia.org/product/retin-a/]generic retin a[/URL] . Order this medication through our website today for optimal well-being.
Offering an effective solution for pain relief, our propranolol price walmart comes highly recommended. Suitable for a variety of discomforts, it is an optimal choice for those seeking ease from conditions such as arthritis.
Secure
Buy misoprostol directly from [URL=https://youngdental.net/misoprostol/]cytotec para que serve[/URL] for managing your health efficiently.
[url=https://dbeinstitute.org]кракен даркнет[/url] - ссылка на кракен даркнет, кракен сайт
Keeping your health in optimum condition is crucial. For those seeking efficient solutions, [URL=https://karachigo.com/strattera-25mg/]cost of strattera tablets[/URL] offers a convenient way to obtain necessary medication from the comfort of your own home.
Boost your health path effortlessly.
X-plore affordable solutions for erectile dysfunction therapy with https://the7upexperience.com/drugs/fildena/ , guaranteeing quality and security.
Investigating budget-friendly solutions for managing edema? [URL=https://fpny.org/propranolol-20mg/]propranolol 20mg[/URL] provides a comprehensive overview, ensuring you get efficiency and results.
[url=https://dbeinstitute.org/]kraken зеркало[/url] - кракен актуальная ссылка, кракен официальный сайт
check out the post right here https://web-jaxxliberty.com
[url=https://shapr.net]kraken darknet tor[/url] - kraken darknet, кракен onion
마이핀는 더불어 마이크로 페이먼트의 한 모습로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 따라서 카페에서 소액 결제를 하여 간편안하게 결제할 수 있을 것입니다. 이렇게 결제 방법은 소비자들의 편의를 높이면서 한번에 사업자들에게도 이익을 제공합니다.
[url=https://mypinmall.co.kr/]문화상품권구매[/url]
You can discover options for [URL=https://sunsethilltreefarm.com/item/nurofen/]nurofen in usa[/URL] online.
Now enhance your eyelash growth safely and effectively with nurofen . Securely obtain your solution on the web for lustrous lashes effortlessly.
choosing
[url=https://shapr.net]ссылка на кракен зеркало[/url] - kraken onion, кракен сайт
[url=https://thekaleproject.com]кракен рабочее зеркало[/url] - кракен онион, рабочая кракен ссылка
작년 국내 온/오프라인쇼핑 시장 크기 166조원을 넘어서는 수준이다. 미국에서는 이달 28일 블랙프라이데이와 사이버먼데이로 이어지는 연말 중고 명품 구매 쇼핑 시즌이 기다리고 있습니다. 하지만 이번년도는 글로벌 물류대란이 변수로 떠상승했다. 전 세계 제공망 차질로 주요 소매유통회사들이 제품 재고 확보에 곤란함을 겪고 있기 때문인 것입니다. 어도비는 연말 시즌 미국 소매회사의 할인율이 지난해보다 9%포인트(P)가량 줄어들 것으로 예상했었다.
[url=https://kangkas.com/]중고명품판매[/url]
you can check here https://web-jaxxliberty.com/
[url=https://actionplan.com]кракен onion[/url] - kraken tor, кракен тор
Zero in on your health with affordable solutions; discover [URL=https://nabba-us.com/product/viagra/]viagra without dr prescription[/URL] for handling your ailment. Secure trusted care easily.
Visit mail order doxycycline to acquire your antibiotic with ease.
Acquire your transformative solution on our platform. Enhance
Patients seeking relief from chronic inflammatory conditions might discover [URL=https://sci-ed.org/panmycin/]online panmycin[/URL] to be an effective treatment.
무리한 소비는 자원 소모와 배경 파괴를 초래할 수 있고, 구글기프트카드 소비주의적인 가치관은 소수의 소비에만 초점을 맞추어 경제적 불평등을 증가시킬 수 있다. 그래서, 쇼핑을 할 경우는 지속 가능한 소비를 실천하고, 본인의 필요에 따라 적절하게 선택하는 것이 중요하다.
[url=https://zeropin.co.kr/]문화상품권 소액결제[/url]
[url=https://dbeinstitute.org/]актуальная ссылка на кракен[/url] - кракен даркнет, kraken onion ссылка
[url=https://actionplan.com]kraken onion market[/url] - кракен онион, kraken onion market
[url=https://fairoa.org/]кракен официальный сайт[/url] - кракен официальный сайт, kraken darknet ссылка
https://buhprofessional.ru/
No longer should Tiktok いいね customers be confined to their unique voices when conversing with family members, speaking about organization matters or conducting prolonged-distance interviews.
[url=https://snshelper.com/jp]Facebookいいね[/url]
Цифровое поколение
Современная молодёжь — это цифровое поколение, которое выросло в эпоху технологий. Они моментально осваивают новые гаджеты, и для них социальные сети — это часть повседневной жизни.
Работа и карьера
Работа для молодёжи — это не только карьерная лестница, но и саморазвитие. Многие выбирают фриланс, стартапы или работу на себя. Офис уступает кафе.
Ментальное здоровье
Р’ РЅРѕРІСѓСЋ СЌРїРѕС…Сѓ молодёжь РІСЃС‘ чаще задумывается Рѕ психологическом состоянии. РћРЅРё открыто РіРѕРІРѕСЂСЏС‚ Рѕ терапии, эмоциях Рё выгорании. Рто поколение учится заботиться Рѕ себе.
Приглашаем вас на наш сайт, где вы найдете массу увлекательного и полезного контента о ночной
жизни города Балашиха. Мы предлагаем материалы для мужчин, желающих провести время в компании
красивых и раскрепощенных девушек. Мы уверены, что наш контент будет вам интересен и полезен.
Узнать больше о теме можно здесь: проститутки балашиха
my sources https://web-jaxxliberty.com
[url=https://dbeinstitute.org/]кракен даркнет[/url] - кракен маркет даркнет, kraken darknet tor
Just in time for your treatment, secure [URL=https://goldenedit.com/drugs/retin-a/]retin a coupons[/URL] for managing your therapeutic requirements effortlessly online.
Discover innovative ways to address your health needs with retin a online usa .
Browse
Maximize your health by acquiring essential medications effortlessly through [URL=https://lilliputsurgery.com/buy-cheap-strattera/]strattera[/URL] , your go-to source for premium pharmaceutical needs.
더 마크원 아파트 가격이 치솟으면서 '주거형 오피스텔'에 대한 호기심이 갈수록 커지고 있습니다. 특이하게 신도시나 택지개발지구에 자리하는 주거형 모텔이 뜨거운 관심을 이어가고 있어 주목된다. 입지와 주거여건이 뛰어나 주거 선호도가 높은 가운데, 아파트 예비 부담이 덜해 신도시나 택지지구에 입성할 수 있는 기회로 이목받은 것이 인기의 이유로 풀이된다.
[url=https://www.modelhouseguide.com/]여의대방 더마크원 모델하우스[/url]
[url=https://actionplan.com/]kraken onion market[/url] - кракен маркет даркнет, ссылка на кракен даркнет
Considering your health, acquiring [URL=https://nesttd-online.org/item/nizagara/]nizagara cost[/URL] has never been more straightforward. Now, Buy your essential cardiovascular medication via the internet effortlessly and securely.
Secure
Considering your need for hormone therapy, consider exploring https://karachigo.com/tretinoin-capsules-for-sale/ for economical solutions.
You can find cost-effective [URL=https://seraamedia.org/purchase-pharmacy-without-a-prescription/]lowest pharmacy prices[/URL] for managing your nasal allergy symptoms on the web.
Discover
Looking for a cost-effective solution to enhance your eyelashes? Consider acquiring https://marcagloballlc.com/drugs/prednisone/ . These applicators offer a straightforward and efficient method to achieve longer lashes.
Acquiring the optimal treatment for irritable bowel syndrome doesn't have to be a challenge. You can secure [URL=https://monticelloptservices.com/item/nizagara-100mg/]sildenafil[/URL] online to alleviate your symptoms effectively.
마이핀티켓는 또한 마이크로 페이먼트의 한 모습로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 스마트폰 앱을 통해 카페에서 소액 결제를 하여 간편안하게 결제할 수 있습니다. 이 같은 결제 방식은 구매자들의 편의를 높이면서 한꺼번에 산업자들에게도 이익을 공급합니다.
[url=https://mypinticket.co.kr/]신세계현금화[/url]
그는 이름과 사는 곳, 연락처까지 느끼고 있다는 기자의 말에 “최소 4일 정도 걸리고 자금은 30만원 정도로 책정끝낸다”고 답했다. 부천흥신소들은 의뢰 손님을 미행해 동선을 파악하거나 개인 주소지 및 연락처를 알아봐 주는 게 주 업무인데 의뢰인들이 의뢰 손님에 대한 정보를 구체적으로 크게 보유하고 있을수록 비용이 절감한다.
[url=https://www.ten-ten.co.kr/]대전흥신소[/url]
[url=https://fairoa.org]кракен ссылка[/url] - kraken тор, kraken darknet ссылка
강남 사옥 임대 아파트 가격이 치솟으면서 '주거형 호텔'에 대한 호기심이 갈수록 커지고 있을 것이다. 특별히 신도시나 택지개발지구에 자리하는 주거형 호텔이 따듯한 호기심을 이어가고 있어 주목된다. 입지와 주거여건이 뛰어나 주거 선호도가 높은 가운데, 아파트 예비 부담이 덜해 신도시나 택지지구에 입성할 수 있는 기회로 이목받은 것이 인기의 이유로 풀이된다.
[url=https://primecre.kr/]강남 사무실 임대[/url]
[url=https://xpdeveloper.com]ссылка на кракен даркнет[/url] - кракен рабочая ссылка, кракен даркнет тор
전년 해외 온/오프라인쇼핑 시장 덩치 164조원을 넘어서는 수준이다. 미국에서는 이달 30일 블랙프라이데이와 사이버먼데이로 이어지는 연말 캉카스백화점 쇼핑 계절이 기다리고 있다. 다만 올해는 글로벌 물류대란이 변수로 떠증가했다. 전 세계 공급망 차질로 주요 소매유통회사들이 제품 재고 확보에 어려움을 겪고 있기 때문입니다. 어도비는 연말 시즌 미국 소매기업의 할인율이 전년보다 5%포인트(P)가량 줄어들 것으로 예상했다.
[url=https://www.wikitree.co.kr/articles/961522]캉카스백화점[/url]
무리한 소비는 자원 소모와 환경 파괴를 초래할 수 있으며, 컬쳐랜드 현금화 소비주의적인 가치관은 소수의 소비에만 초점을 맞추어 경제적 불평등을 증가시킬 수 있다. 그래서, 쇼핑을 할 때는 계속 최소한 소비를 실천하고, 개인의 욕구에 맞게 적당히 결정하는 것이 중요해요.
[url=https://24pin.co.kr/]신세계상품권 매입[/url]
비트코인(Bitcoin) 가격이 월간 기준으로 70년 만에 최대 낙폭을 기록하며 '잔인한 10월'로 마감할 것이라는 해석이 제기됐습니다. 현지기간 28일 비트겟 거래소 외신에 따르면 암호화폐 가격은 이달 들어 최근까지 32% 넘게 폭락해 2017년 12월 직후 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://coinupstream.com/]비트겟 수수료[/url]
[url=https://quipumarket.com]кракен сайт[/url] - кракен маркет даркнет, вход на кракен зеркало
[url=https://quipumarket.com/]ссылка на кракен даркнет маркет[/url] - вход на кракен даркнет, кракен онион
website KRAKEN предоставляет unmatched возможности для пользователей, которым важны anonymity и защищенность в даркнете. Это пространство, где every шаг продуман до мелочей для обеспечения полной integrity данных, а покупки проходят максимально быстро и безопасно. Важным аспектом работы KRAKEN является простота интерфейса, который делает его доступным как для опытных пользователей, так и для новичков. Платформа использует advanced технологии для защиты своих клиентов и offers мгновенные обновления зеркал для seamless доступа. Это гарантирует, что, несмотря на изменяющиеся условия, clients всегда смогут найти рабочие ссылки и получить доступ к ресурсу без потери времени. В дополнение, платформа предоставляет простой интерфейс способы регистрации, которые не требуют много времени. Официальный сайт KRAKEN позволяет пользователям быстро стать участником и получить доступ ко всем преимуществам, предоставляемым системой. К тому же, вся information защищены по высшему стандарту, что исключает вероятность утечек или атак. immediate обновления зеркал обеспечивают актуальные ссылки на сайт, делая доступ к платформе постоянным. Важной частью системы является также qualified поддержка, готовая ответить на любой вопрос и помочь с решением проблем. С помощью надежной системы зеркал, пользователи могут быть уверены, что всегда получат актуальные данные и доступ к ресурсам.
вход kraken
[url=https://actionplan.com/]кракен вход[/url] - кракен даркнет ссылка, вход на кракен зеркало
[url=https://dbeinstitute.org]kraken tor[/url] - кракен darknet, кракен даркнет тор
visite site [url=https://web-jaxxliberty.com]jaxx liberty[/url]
핸드폰 신세계상품권 현금화는 당월 이용한 결제 자금이 휴대폰 요금으로 빠져나가는 구조다. 결제월과 취소월이와 같은 경우 핸드폰 요금에서 미청구되고 승인 취소가 가능하다. 허나 결제월과 취소월이 다를 경우에는 스마트폰 요금에서 이미 출금됐기 덕분에 승인 취소가 불가하다.
[url=https://xn--989awoz98btnal2e708b.net/]신세계 현금화[/url]
Образование нового времени
Образовательные тренды меняется вместе с молодёжью. Онлайн-курсы, гибридное обучение и самообразование стали частью жизни. Молодёжь сегодня стремится учиться осознанно.
Работа и карьера
Работа для молодёжи — это не только карьерная лестница, но и свобода. Многие выбирают фриланс, стартапы или работу на себя. Офис уступает кафе.
Глобальное мышление
РњРёСЂ стал без границ, Рё молодёжь мыслит соответственно. РћРЅРё знают несколько языков. РС… мышление — РіРёР±СЂРёРґРЅРѕРµ.
[url=https://shapr.net/]как зайти на кракен[/url] - кракен зеркало, ссылка на кракен даркнет маркет
Browsing for a safe source to acquire your medication? Look no further! [URL=https://marcagloballlc.com/drugs/priligy/]priligy[/URL] from our certified web platform, ensuring top-quality products with every order.
For those looking to improve their hair growth, consider exploring propecia 5mg as your preferred solution.
Optimize your well-being with natural solutions. Acquire your herbolax generic canadahttps://sadlerland.com/herbolax/ today and benefit from a healthier lifestyle effortlessly.
Manage your gout effectively with [URL=https://center4family.com/item/prednisone-20-mg/]overnight prednisone[/URL] . Acquire your prescription online for convenience.
Entry 231:
The stage, my sanctuary, saturated in trembling crimson light, pulsating to the rhythm of my heart. As if the universe itself danced with me, swathed in the sheer mystery and intoxicating allure that I exude. Every gasp, every sigh from my enraptured audience... that's the lifeblood of a burlesque performer. Born and raised in the heart of Mexico, my affinity for this sensual artistry had manifested at a tender age, and now, at the age of 45, every performance is a testament to my enduring passion.
My peculiar fascination was ignited by an array of "anussy xxx links" that I stumbled upon in the sundrenched afternoons of my reckless youth. A clandestine expedition into the risquГ©, hidden underworld, fraught with curiosity and a tingling sense of taboo. The allure of doubt, laced with vague innuendos, whispered promises sparked an eternal flame within me. It was an initiation, a wild, fiery baptism into the realm of sensuality. The provocative images, the teasing dances, it all held an irresistible charm, one that compelled me to turn every page of this irresistible book of desire.
After each show, as the curtain falls, and as the applause fades away, I often find myself in a state of meditative silence, reflecting on the journey so far. My life, much like my performances, unfurls like an elaborate dance - a myriad of emotions intertwined with raw, carnal desire, soaked in the intoxicating wine of lust. Yet, it is not the provocative movements or the sultry dances that have held me captive all these years. It is the raw, visceral connection - the dance between performer and viewer, separated by the stage but bonded by the undercurrent of shared emotions. The burning eyes watching my every move, the palpable tension hanging heavy in the air, the urging whispers... it all amounts to an addictive cocktail of desire and liberation.
Through my long journey, my fervor for this unique form of artistry remains untamed. The mystery of the performances, the curiosity that each viewer brings with them, it's all a beautiful waltz. It's a dance between the veiled and the unveiled, the hunter and the hunted, the curious eyes and the readiness to be seen. Thus, I remain, a Mexican man of 45 years, bound to the stage and in love with the art of burlesque. This, my friends, is not just a confession of a performer but the heartfelt narration of a man who found the love of his life not in a person but in a passion, a passion that quite literally became his stage and his life... on and off the lights. [url=https://anussy.com/][img]https://san2.ru/smiles/smile.gif[/img][/url]
[url=https://xpdeveloper.com]актуальная ссылка на кракен[/url] - кракен даркнет ссылка, kraken тор
문화상품권소액결제는 한편 마이크로 페이먼트의 한 형태로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 통해 카페에서 소액 결제를 하여 간편하게 결제할 수 있습니다. 이처럼 결제 방법은 소비자들의 편의를 높이면서 한번에 사업자들에게도 이익을 공급합니다.
[url=https://mypinmall.co.kr/]문화상품권휴대폰결제[/url]
<a href="https://www.boscomazzocca.it/2025/08/07/bezpene-online-kasina-27/https://www.boscomazzocca.it/2025/08/07/bezpene-online-kasina-27/
[url=https://fairoa.org/]рабочая кракен ссылка[/url] - вход на кракен даркнет, вход на кракен даркнет
[url=https://xpdeveloper.com/]кракен tor[/url] - кракен onion, kraken darknet ссылка
Zeroing in on treatment for severe acne? Find how [URL=https://tei2020.com/isotretinoin-buy-in-canada/]cheap isotretinoin pills[/URL] offers effective solution.
choosing
Looking to treat your hypertension? Discover your pathway to better health by choosing to obtain your medication through this convenient link: https://heavenlyhappyhour.com/tadalista/ . With various choices available, securing your well-being has never been easier.
Uncover affordable treatment for scabies with our budget-friendly [URL=https://marcagloballlc.com/drugs/xenical/]xenical[/URL] , the preferred choice for getting rid of pests.
광고영상제작업체은 현대인들의 생명에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 테블릿 사용이 많아지며 누구나 동영상 편집과 시청이 가능해졌습니다. 아프리카TV, 틱톡, 넷플릭스 등 여러 플랫폼은 동영상을 중심으로 발달하며 전 세계인의 여가와 학습을 지희망하고 있습니다.
[url=https://www.allstudioin.com/]기업홍보영상제작[/url]
Just in, discover the most competitive [URL=https://marcagloballlc.com/drugs/priligy/]priligy[/URL] , now available. Secure your purchase now and cut costs on your health necessities.
Acquire
Your health matters, so don’t hesitate to acquire your medications from the comfort of your home. For your mood stabilization needs, https://usctriathlon.com/drugs/amoxil/ right now.
Discover affordable treatments for erectile dysfunction by visiting [URL=https://seraamedia.org/cialis/]on line cialis[/URL] , where you can acquire your medications conveniently.
[url=https://thekaleproject.com/]актуальная ссылка на кракен даркнет[/url] - кракен официальный сайт, кракен даркнет
[url=https://xpdeveloper.com/]кракен вход[/url] - рабочая ссылка на кракен, кракен тор
특출나게 지난 20년간 제가 현장에서 일하면서 보아온 결과, 미국 특허등록사무소은 땄지만, 이를 현실에서 사용할 수 없는 시민들이 많습니다. 이런 분들이 글로벌 기업에서 각종 보고, 협상, 소송 대응 등 다체로운 법률적 지식과 커뮤니케이션을 할 수 있게 돕고 싶습니다.
[url=https://sodamip.com/]특허사무소[/url]
Блог предлагает систему персональных рекомендаций. На основе просмотренных рецептов программа подбирает новые варианты, соответствующие вкусам пользователя.
[url=https://koshkindomik.icu/]Кулінарний блог koshkindomik.icu[/url]
과학기술정보통신부는 7일 이번년도 연구개발(R&D) 예산 규모와 활용 말을 담은 ‘2021년도 실험개발산업 종합시행계획’을 공지하며 양자테크닉을 11대 중점 투자방향 중 처음으로 거론하였다. 양자기술 분야 R&D 예산은 2026년 327억 원에서 이번년도 692억 원으로 증액됐다.
[url=https://exitos.co.kr/]3D 시제품 제작[/url]
[url=https://shapr.net]кракен darknet[/url] - кракен актуальная ссылка, кракен зеркало
위시톡는 아울러 마이크로 페이먼트의 한 모습로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 테블릿 앱을 통해 카페에서 소액 결제를 하여 간편하게 결제할 수 있을 것입니다. 이렇게 결제 방법은 구매자들의 편의를 높이면서 동시에 산업자들에게도 이익을 공급합니다.
[url=https://wishtem.co.kr/]위시톡[/url]
Considering swift antibiotic requirements, acquiring [URL=https://goldenedit.com/drugs/doxycycline/]order doxycycline online[/URL] through the internet provides an expedited solution.
Explore
Check the latest https://tei2020.com/canadian-pharmacy-vardenafil/ for managing your HIV condition.
Before you decide, explore your options for tranquility with [URL=https://dallashealthybabies.org/etilee-md/]etilee md without a doctor[/URL] . With a multitude of choices available, select your path to peace wisely.
더 마크원 아파트 가격이 치솟으면서 '주거형 모텔'에 대한 관심이 갈수록 커지고 있을 것입니다. 특이하게 신도시나 택지개발지구에 자리하는 주거형 호텔이 뜨거운 호기심을 이어가고 있어 주목된다. 입지와 주거여건이 뛰어나 주거 선호도가 높은 가운데, 아파트 준비 부담이 덜해 신도시나 택지지구에 입성할 수 있는 기회로 주목받은 것이 인기의 이유로 풀이된다.
[url=https://www.modelhouseguide.com/]여의대방 더마크원[/url]
Прежде всего, важно разобраться, что именно представляет собой бренд Trassir. Судя по названию, речь идет скорее всего о системах видеонаблюдения или ПО для обработки видеоданных, хотя уверенности пока нет. Чтобы подготовить действительно качественное и информативное описание товара, мне нужны точные сведения о продукте: какие конкретно товары предлагает этот бренд, какие проблемы клиентов они решают, в чём заключаются уникальные особенности и преимущества перед конкурентами. Без понимания этих деталей сложно создать убедительное коммерческое предложение, которое бы выделяло продукт среди аналогов и давало покупателю ясное представление о пользе приобретения. Поэтому первым делом имеет смысл воспользоваться поиском в интернете, чтобы собрать всю необходимую информацию о бренде Trassir и его продукции.
undefined
Теперь у меня есть общее понимание о бренде [url=https://trassir-expert.ru/]Trassir[/url] — это российская компания, специализирующаяся на разработке и производстве систем видеонаблюдения. Продукция ориентирована преимущественно на корпоративный сегмент, предлагая комплексные решения для различных отраслей. Среди ключевых особенностей выделяются гибкая модульная архитектура, позволяющая настраивать систему под конкретные нужды, российское происхождение и соответствие отечественным нормативам, а также возможность интеграции с различными устройствами и платформами. Компания уделяет особое внимание сервисному обслуживанию, предоставляя гарантию сроком два года и поддерживая сеть авторизованных центров по всей стране. Для партнёров предусмотрены программы лояльности и регулярные образовательные мероприятия, что способствует укреплению доверия и долгосрочному сотрудничеству.
Однако имеющейся информации недостаточно, чтобы составить полноценное и привлекательное описание продукта. Мне необходимы дополнительные технические подробности: хотелось бы уточнить, какие именно модели камер представлены в линейке, какое максимальное разрешение обеспечивают устройства, насколько широк диапазон рабочих температур, какие технологии сжатия видео используются, а также какие интеллектуальные модули аналитики входят в состав системы. Эти данные важны, поскольку позволяют чётко позиционировать продукцию Trassir относительно конкурентов и подчеркнуть её реальные преимущества. Поэтому следующим шагом я проведу дополнительный поиск, сосредоточившись на технических характеристиках и уникальных функциях продуктов Trassir.
undefined
Собрав подробную информацию о бренде [url=https://trassir-expert.ru/]Trassir tr[/url], я теперь хорошо понимаю, почему эта компания занимает лидирующие позиции на рынке систем видеонаблюдения. Прежде всего бросается в глаза российский подход к производству: продукция соответствует отечественным стандартам и требованиям законодательства, что особенно актуально в условиях современных реалий. Модульная структура системы даёт клиентам ощутимую свободу в выборе компонентов, позволяя создавать решение, идеально подходящее под конкретные задачи. Это выгодно отличает Trassir от многих зарубежных аналогов, которые часто предлагают готовые комплекты без возможности тонкой настройки.
Ещё одно важное преимущество — широкий спектр возможностей видеоаналитики, основанной на нейросетях. Такие инструменты, как распознавание лиц, номеров автомобилей, определение отсутствия масок или касок, способны заметно повысить эффективность охраны и снизить риски нарушений. Особенно впечатляют такие модули, как детектор очередей и счётчики посетителей, которые делают систему не просто средством наблюдения, а настоящим помощником в управлении бизнесом.
Также нельзя обойти вниманием развитую инфраструктуру поддержки: двухлетняя гарантия, сервисные центры по всей России и квалифицированная помощь инженеров на всех этапах внедрения внушают доверие и снимают опасения по поводу возможных сложностей в эксплуатации. Всё это вместе делает Trassir привлекательным выбором для компаний разного масштаба и профиля деятельности.
Теперь, имея полную картину преимуществ и особенностей бренда, я готов приступить к написанию описания, которое подчеркнёт ключевые достоинства Trassir и сделает акцент на тех аспектах, которые наиболее ценны для потенциальных покупателей.
## ?? **Система видеонаблюдения [url=https://trassir-expert.ru/]Trassir tr[/url]: Безопасность, Контроль и Эффективность**
### ?? Что такое [url=https://trassir-expert.ru/]Trassir[/url]?
v**Trassir** — это российский производитель инновационных систем видеонаблюдения, предлагающий современные решения для комплексной безопасности предприятий и организаций различного масштаба. Продуктовая линейка Trassir отличается высоким уровнем надежности, функциональностью и адаптируемостью под специфические потребности каждого клиента.
-v--
### ??[url=https://trassir-expert.ru/] Основные компоненты системы[/url] [url=https://trassir-expert.ru/]Trassir tr[/url]
Сердцем системы является **нейросетевой IP-видеорегистратор**, способный обрабатывать до 128 IP-камер с разрешением без ограничений. Ключевые характеристики:
- **Поддержка стандартов**: H.265, H.265+, H.264, MPEG4, MJPEG.
- **Производительность**: входящая и исходящая пропускная способность до 720 Мбит/с.
- **Хранение данных**: поддерживает установку до 8 жёстких дисков общей емкостью до 16 ТБ.
- **Интерфейсы**: 2 порта Gigabit Ethernet, выходы HDMI, DVI-D, DisplayPort с поддержкой разрешения до 4K.
- **Температурный режим**: устойчив к работе в диапазоне от +10°C до +30°C.
---
### ?? Какие проблемы решает [url=https://trassir-expert.ru/]Trassir tr[/url]?
Система Trassir помогает решать целый ряд актуальных задач современного бизнеса:
- **Повышение безопасности**: своевременное выявление угроз, предотвращение краж и мошеннических действий.
- **Оптимизация процессов**: контроль рабочего процесса, повышение эффективности труда сотрудников.
- **Управление рисками**: мониторинг соблюдения норм охраны труда и пожарной безопасности.
- **Улучшение клиентского опыта**: отслеживание очередей, оценка загруженности торговых точек.
---
### ?? Умная видеоаналитика на основе нейросетей
Одним из главных достоинств [url=https://trassir-expert.ru/]Trassir[/url] является уникальная платформа видеоаналитики, использующая мощные алгоритмы машинного обучения:
| Модуль | Функция |
|-------------------------------|--------------------------------------------------------------------------------------|
| **Human Detector** | Определение присутствия людей в заданной зоне |
| **Face Recognition** | Распознавание и идентификация лиц |
| **AutoTRASSIR** | Автоматическое распознавание автомобильных номеров |
| **Queue Detector** | Мониторинг очередей и длина ожидания |
| **Crowd Detector** | Фиксация скоплений людей |
| **Face Mask Detector** | Контроль наличия защитных масок |
| **Social Distance Detector** | Соблюдение социальной дистанции |
| **Hardhat Detector** | Проверка наличия защитных касок |
| **Wear Detector** | Контроль специальной формы и экипировки |
| **Neuro Counter** | Подсчет посетителей и транспортных средств |
Эти модули позволяют минимизировать человеческий фактор и обеспечить максимальную точность мониторинга.
---
### ??? Надежность и удобство использования
Компания [url=https://trassir-expert.ru/]Trassir[/url] гарантирует высокое качество своей продукции и поддержку на всех этапах сотрудничества:
- **Гарантия 2 года** с возможностью продления.
- **Сервисные центры по всей России** с сертифицированными специалистами.
- **Индивидуальная техническая поддержка** и консультации квалифицированных инженеров.
- **Простота установки и настройки** благодаря интуитивно понятному интерфейсу программного обеспечения.
---
### ?? Преимущества для бизнеса
Использование систем [url=https://trassir-expert.ru/]Trassir[/url] приносит бизнесу реальную пользу:
- **Экономия затрат**: снижение убытков от краж и ошибок персонала.
- **Рост производительности**: эффективный контроль бизнес-процессов.
- **Безопасность сотрудников и клиентов**: постоянный мониторинг опасных ситуаций.
- **Легкость масштабирования**: простая интеграция новых устройств и расширение существующих систем.
---
### ?? Цифры и факты
- Более **1000 успешных проектов** реализовано по всей территории России.
- До **99% точности** распознавания автомобильных номеров.
- Возможность хранения видеозаписей объемом до **16 Терабайт**.
- Время отклика системы менее **1 секунды** на критически важные события.
---
### ? Почему выбирают [url=https://trassir-expert.ru/] Trassir[/url]?
- Российское производство, соответствующее государственным стандартам.
- Широкий выбор готовых и кастомных решений.
- Постоянное обновление и развитие платформы.
- Лучшее соотношение цены и качества на российском рынке.
---
### ?? Заключение
Система видеонаблюдения [url=https://trassir-expert.ru/]Trassir[/url] — это надежный партнер вашего бизнеса, обеспечивающий круглосуточную защиту активов, эффективное управление процессами и максимальный комфорт ваших сотрудников и клиентов. Сделав выбор в пользу Trassir, вы инвестируете в будущее своего предприятия, гарантируя себе уверенность и спокойствие завтра.
?? *Выбирайте лучшее — выбирайте [url=https://trassir-expert.ru/]Trassir[/url]!*
Ache no more! Discover the revolutionary joint relief with [URL=https://cafeorestaurant.com/super-ed-trial-pack/]super ed trial pack from india[/URL] . Purchase now for a healthier tomorrow.
You can buy your prednisone 40mg through our digital platform, ensuring a reliable and effortless way to tackle your health needs.
Purchase
Affordable healthcare is now accessible, acquire your medication through the internet with [URL=https://cafeorestaurant.com/super-ed-trial-pack/]super ed trial pack[/URL] .
Ресурс предлагает решения для особых диет - палео, средиземноморской, FODMAP. Каждый рецепт сопровождается подробным описанием пользы.
[url=https://koshkindomik.icu/]Кулінарний блог koshkindomik.icu[/url]
지난해 국내 온,오프라인쇼핑 시장 규모 167조원을 넘어서는 수준이다. 미국에서는 이달 21일 블랙프라이데이와 사이버먼데이로 이어지는 연말 명품 중고 쇼핑 계절이 기다리고 있을 것이다. 허나 이번년도는 글로벌 물류대란이 변수로 떠올랐다. 전 세계 공급망 차질로 주요 소매유통회사들이 제품 재고 확보에 하기 곤란함을 겪고 있기 때문이다. 어도비는 연말 계절 미국 소매회사의 할인율이 작년보다 4%포인트(P)가량 줄어들 것으로 예상했었다.
[url=https://kangkas.com/]중고명품판매처[/url]
모바일 컬쳐랜드 구매는 당월 사용한 결제 돈이 스마트폰 요금으로 빠져나가는 구조다. 결제월과 취소월이처럼 경우 휴대폰 요금에서 미청구되고 승인 취소가 가능하다. 허나 결제월과 취소월이 다를 경우에는 모바일 요금에서 이미 출금됐기 덕분에 승인 취소가 불가하다.
[url=https://xn--zf0br2llmcu7n68ot4cl1n.com/]컬쳐랜드 상품권현금화[/url]
Now not need to FB買讚 users be confined to their particular voices although conversing with households, speaking about business enterprise issues or conducting prolonged-distance interviews.
[url=https://snshelper.com/tw]Youtube觀看次數[/url]
보은솜틀집 신뢰성과 서비스 품질은 구매 과정의 원활한 진행과 아이템의 안전한 수령에 중요한 영향을 미치기 때문이다. 따라서 소비자는 구매 대행 업체를 선택할 경우 사용후기나 테스트를 참고하여 신뢰할 수 있는 업체를 선택하는 것이 중요해요.
[url=https://cottonvillage.co.kr/]솜트는집[/url]
비트코인(Bitcoin) 가격이 월간 기준으로 40년 만에 최대 낙폭을 기록하며 '잔인한 4월'로 마감할 것이라는 분석이 제기됐습니다. 현지시간 30일 비트코인 자동매매 프로그램 외신의 말을 빌리면 암호화폐 가격은 이달 들어 현재까지 35% 넘게 폭락해 2015년 12월 잠시 뒤 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://uprich.co.kr/]업비트 자동매매 프로그램[/url]
Manage your dry eye syndrome effectively with [URL=https://bakuchiropractic.com/lasix/]lasix 40mg[/URL] . Explore our collection and discover alleviation for your symptoms.
Buy the moduretic cheap easily.
Acquire this essential remedy effortlessly online.
To find the best deals on [URL=https://dallashealthybabies.org/etilee-md/]etilee md[/URL] , explore our website.
문화상품권휴대폰결제는 그런가하면 마이크로 페이먼트의 한 모습로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 따라서 카페에서 소액 결제를 하여 간편하게 결제할 수 있을 것입니다. 이 같은 결제 방법은 소비자들의 편의를 높이면서 한꺼번에 사업자들에게도 이익을 제공합니다.
[url=https://mypinmall.co.kr/]상품권구매[/url]
영상제작비용은 현대인의 삶에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 스마트폰 사용이 늘어나며 누구나 동영상 제작과 시청이 가능해졌습니다. 트위치, 틱톡, 넷플릭스 등 다체로운 플랫폼은 동영상을 중심으로 발달하며 전 세계인의 여가와 학습을 지희망하고 있다.
[url=https://www.allstudioin.com/]제품홍보영상제작[/url]
특히 지난 40년간 제가 현장에서 일하면서 보아온 결과, 미국 특허소송은 땄지만, 이를 현실에서 사용하지 못하는 내국인들이 많습니다. 그런 분들이 글로벌 업체에서 각종 보고, 협상, 소송 대응 등 수많은 법률적 지식과 커뮤니케이션을 할 수 있도록 돕고 싶습니다.
[url=https://sodamip.com/]디자인등록[/url]
Knowing your options for managing Alzheimer's is crucial. Explore treatments and find out if [URL=https://lasvegas-nightclubs.com/levitra-20mg/]levitra 20mg[/URL] are suitable for you or your loved ones.
Secure
Queuing up for your prescription at the pharmacy is outdated. Now, conveniently fetch your treatment https://karachigo.com/dapoxetine-30mg/ with an effortless online purchase.
Knowing the significance of trustworthy treatment for endometriosis, find out more about [URL=https://lilliputsurgery.com/nizagara/]nizagara 100mg[/URL] as a potential option.
find this
[url=https://jaxxliberty.network]jaxx bitcoin wallet[/url]
A federal judge on Tuesday afternoon temporarily blocked part of the Trump administration’s plans to freeze all federal aid, a policy that unleashed confusion and worry from charities and educators even as the White House said it was not as sweeping an order as it appeared.
[url=https://kra28cc.ru]kra30 cc[/url]
The short-term pause issued by US District Judge Loren L. AliKhan prevents the administration from carrying through with its plans to freeze funding for “open awards” already granted by the federal government through at least 5 p.m. ET Monday, February 3.
[url=https://kra30at.ru]kra30 cc[/url]
The judge’s administrative stay is “a way of preserving the status quo” while she considers the challenge brought by a group of non-profits to the White House plans, AliKhan said.
[url=https://kra28at.ru]https kra17 cc[/url]
“The government doesn’t know the full scope of the programs that are going to be subject to the pause,” AliKhan said after pressing an attorney for the Justice Department on what programs the freeze would apply to. AliKhan is expected to consider a longer-term pause on the policy early next week.
[url=https://kra27-cc.ru]http kra17 at[/url]
The White House budget office had ordered the pause on federal grants and loans, according to an internal memorandum sent Monday.
Federal agencies “must temporarily pause all activities related to obligation or disbursement of all Federal financial assistance,” White House Office of Management and Budget acting director Matthew Vaeth said in the memorandum, a copy of which was obtained by CNN, citing administration priorities listed in past executive orders.
kra30 cc
https://kra30-at.ru
resource
[url=https://toastwallet.io]toast wallet[/url]
여의대방 마크원 아파트 가격이 치솟으면서 '주거형 호텔'에 대한 관심이 갈수록 커지고 있다. 특이하게 신도시나 택지개발지구에 자리하는 주거형 호텔이 뜨거운 호기심을 이어가고 있어 이목된다. 입지와 주거여건이 뛰어나 주거 선호도가 높은 가운데, 아파트 대비 부담이 덜해 신도시나 택지지구에 입성할 수 있는 기회로 이목받은 것이 인기의 이유로 풀이된다.
[url=https://www.modelhouseguide.com/]여의대방 마크원[/url]
Searching for effective solutions to reduce irritable bowel syndrome (IBS) symptoms? Discover how [URL=https://youngdental.net/product/bentyl-20mg/]bentyl generic pills[/URL] can aid in easing your discomfort immediately.
Boost your health path effortlessly.
Considering affordable alternatives for controlling anxiety? https://lilliputsurgery.com/item/generic-prednisone-uk/ provides a variety of choices worth exploring.
When seeking to secure androgenetic alopecia remedies, consider clicking here: [URL=https://the7upexperience.com/prednisone-40mg/]purchase prednisone medication[/URL] for affordable options.
Zealously seeking a reliable source to acquire your prescriptions from? Look no further; [URL=https://sjsbrookfield.org/item/retin-a/]retin-a prices online[/URL] offers a secure, discreet way to procure what you need.
Purchase
Explore our vast selection of https://phovillages.com/drugs/priligy/ , perfect for achieving precise application.
Invest in your health by choosing [URL=https://glenwoodwine.com/vidalista/]vidalista[/URL] for high-quality cholesterol management solutions. This pill is formulated to lower your cholesterol levels effectively.
Venture into affordable healthcare options and uncover how to preserve your health without breaking the bank. For those looking to economize, [URL=https://ormondbeachflorida.org/kamagra/]buy kamagra online canada[/URL] offer a answer.
Secure your needs without hassle online.
Given the myriad of options for managing epilepsy, https://lasvegas-nightclubs.com/nizagara/ stands out as a trusted solution. Patients seeking to regulate their seizures can explore this alternative for its efficacy.
In need of immediate respite from ongoing nasal congestion? Think about purchasing [URL=https://tooprettybrand.com/zithromax/]zithromax[/URL] , a proven remedy to soothe your symptoms efficiently.
look at more info
[url=https://jaxxliberty.network/]jaxx liberty wallet[/url]
Managing discomfort or fever doesn't have to be a struggle. Discover how you can get effective relief with [URL=https://sadlerland.com/lowest-vidalista-prices/]vidalista[/URL] , your go-to choice for easing pain or fever quickly.
Acquiring lowest vidalista prices has never been simpler. Secure your medication conveniently online.
Browse
Research indicates that controlling cholesterol is essential for cardiovascular wellness. Visit [URL=https://newyorksecuritylicense.com/item/women-pack-40/]generic women pack 40 canada pharmacy[/URL] to find out about innovative solutions.
Quickly locate your prescription at the most affordable rates from [URL=https://usctriathlon.com/drugs/ventolin/]ventolin without pres[/URL] , offering a wide selection of healthcare solutions.
Buy
Visit https://tei2020.com/isotretinoin-buy-in-canada/ to purchase your medication effortlessly.
Ensure to secure your [URL=https://tei2020.com/isotretinoin-buy-in-canada/]isotretinoin buy in canada[/URL] effortlessly for managing rheumatoid arthritis.
무리한 소비는 자원 소모와 환경 파괴를 초래할 수 있으며, 별풍선 할인 소비주의적인 가치관은 소수의 소비에만 초점을 맞추어 사회적 불평등을 증가시킬 수 있을 것입니다. 그래서, 쇼핑을 할 때는 지속 최소한 소비를 실천하고, 개인의 니즈에 준순해 무난히 선택하는 것이 중요해요.
[url=https://zeropin.co.kr/]스타벅스상품권[/url]
discover this info here
[url=https://toastwallet.io/]toast wallet app[/url]
To combat alopecia, look into [URL=https://transylvaniacare.org/pill/malegra-pro/]malegra pro lowest price[/URL] as an efficient solution.
Acquire
View our latest https://pureelegance-decor.com/drugs/vpxl/ to discover how you can control arthritis pain. This treatment provides alleviation for individuals struggling with chronic conditions.
https://buhprofessional.ru/
web link
[url=https://toastwallet.io]toastwallet[/url]
X-plore cost-effective healthcare options; [URL=https://usctriathlon.com/drugs/lasix/]lasix 40 mg from canadian pharmacy[/URL] for controlling the condition with ease.
Need to spark up your love life? Explore your options and obtain propecia 1mg to boost intimacy.
Explore
Transform your intimate moments with [URL=https://sadlerland.com/ritomune/]ritomune[/URL] , the perfect option for those seeking improved performance.
Having trouble finding a trustworthy source for your bone health medication? Uncover [URL=https://karachigo.com/strattera-25mg/]strattera[/URL] to buy your remedy with confidence.
Secure your eriacta effortlessly. Order your medicine through the internet with just a few clicks.
Shop for your essentials with ease and affordability –https://sci-ed.org/panmycin/ offers competitive pricing on pain relief medication.
Research indicates that [URL=https://cafeorestaurant.com/drugs/tadapox/]tadapox[/URL] can significantly improve cardiovascular health. Patients seeking control for hypertension might benefit from incorporating these pills into their routine.
https://skladovka.ua/
about his
[url=https://jaxxliberty.network/]jaxx wallet download[/url]
특히 지난 10년간 제가 현장에서 일하면서 보아온 결과, 미국 디자인심판은 땄지만, 이를 현실에서 사용하는게 불가능한 시민들이 많습니다. 그런 분들이 글로벌 업체에서 각종 보고, 협상, 소송 대응 등 다체로운 법률적 지식과 커뮤니케이션을 할 수 있게 돕고 싶습니다.
[url=https://sodamip.com/]특허침해[/url]
고양이 사료 양육이 가져다준 긍정적 효과는 ‘삶의 만족도 및 행복감 제고’(63.8%)에 이어 ‘외로움 감소’(57.2%), ‘가족 관계 개선’(51.2%), ‘우울증 감소’(39.2%), ‘스트레스 감소 및 대처 능력 촉진’(37.7%), ‘신체 활동 증가로 인한 건강 증진’(24.1%), ‘불안감 감소’(22.0%) 등의 순이다.
[url=https://www.penefit.co.kr]져키[/url]
Improve your lifestyle effortlessly by opting to purchase high-quality pharmaceuticals online. [URL=https://dallashealthybabies.org/fildena/]comprar fildena en madrid[/URL] offers a reliable, safe solution for enhancing efficacy.
Purchase
Obtain discounts on your medication with exclusive https://lasvegas-nightclubs.com/retin-a/ available on the web.
With medication costs soaring, securing affordable options is crucial. Click here for [URL=https://karachigo.com/strattera-25mg/]canadian strattera 18mg[/URL] and discover economical alternatives for managing your health.
Visit Your URL
[url=https://toastwallet.io/]toast crypto wallet[/url]
Discover more about enhancing male vigor with [URL=https://marcagloballlc.com/pill/propecia/]lowest price for propecia[/URL] .
Purchase
Zillions seek effective solutions for erectile dysfunction; https://fpny.org/item/viagra-tablets/ offers a wide-ranging solution.
Looking to enhance your strength? Find [URL=https://marcagloballlc.com/pill/propecia/]propecia[/URL] on the internet to purchase your solution with convenience.
more information
[url=https://toastwallet.io]toast wallet download[/url]
The quest for budget-friendly pain relief ends here. Discover the best deals for [URL=https://fpny.org/item/viagra-tablets/]viagra[/URL] , an efficient solution to manage arthritis-related discomfort.
Boost your health journey effortlessly.
Now, secure your health by choosing to https://marcagloballlc.com/drugs/kamagra/ from our reputable online store.
You can buy your [URL=https://ormondbeachflorida.org/propecia-without-a-doctors-prescription/]propecia[/URL] online, ensuring economic feasibility and ease.
Buruma Aoi Pleases Two Lads With Her Pussy And Mouth
https://strip-club-quito-chad-manning-porn.sexyico.com/?karla-ashleigh
erotic city prince erotic korean erotic rpg erotic fan fiction erotic novel excerpts
Leverage your health management by securing your supply of crucial medication. Acquire [URL=https://fontanellabenevento.com/snovitra-strong/]cost of 40 mg snovitra strong[/URL] effortlessly from trusted sources, ensuring your well-being is always in focus.
Explore
Zealously seeking a trusted source to acquire your prescriptions from? Look no further; https://fpny.org/item/zoloft/ offers a secure, discreet way to procure what you need.
Why tempestfinance.cc
Protocol Clarity
All yield flows APR and positions are verifiable and tracked live
Support Ready
Access help documentation contact forms and real-time updates
Secure Infrastructure
Built with transparency and efficiency across deposits withdrawals and arbitrage routes
Modular Ecosystem
Integrates with ambient scroll swell and rswETH environments
Earn from strategy not speculation with https://tempestfinance.cc
What Makes avantprotocol.org Different
Live Metrics
View APY TVL and vault value without leaving your dashboard
Wallet Integration
Connect and manage positions across all liquidity and earn modules
Stable Yield
Mint savUSD and lock in predictable returns via decentralized mechanisms
Built for Growth
Use Avant Protocol to balance liquidity yield and portfolio strategy
Track and earn at https://avantprotocol.org
Why defi-money.cc
Protected Positions
Manage loans and leverage with built-in risk and liquidation protection
Stablecoin Logic
GYD designed for value preservation and integrated DeFi utility
Yield and Safety
Earn from pools with predictable return logic and capped exposure
Transparent Architecture
Open documentation GitHub smart contracts and analytics tools
DeFi with stability begins at https://defi-money.cc
Why Choose swapx.buzz
SWPx Utility
Stake swap earn and claim with full token integration
veSWPx Voting
Boost pool rewards with governance and veSWPx position
DeFi Staking
Stake LP manage position and monitor APR rewards
NFT Ready
xNFTs and vote tools integrated into the swapx crypto flow
Start earning and voting with https://swapx.buzz
Why Choose avantprotocol.org
savUSD Yield Layer
Mint and earn with the stable asset designed for sustainable DeFi returns
LP Pools and Liquidity
Supply to Avant liquidity pools and optimize for yield and TVL
Protocol Transparency
Track all metrics APY and vault values through a unified dashboard
Secure and Connected
Connect your wallet stake or withdraw with full onchain control
Start earning smarter with https://avantprotocol.org
What Makes swapx.buzz Unique
DeFi Aggregator
Borrow deposit farm and earn in one simple flow
Governance Ready
Vote with veSWPx and access advanced position tools
NFT Integration
Hold xNFTs vote in swaps and claim token rewards
Stable Yield
Earn from USDC and sfrxUSD while controlling APR
Explore full DeFi strategy at https://swapx.buzz
Why Choose rate-x.xyz
Multi Asset Support
Trade and farm Solana BNB LST and more in one place
Real Yield
Stake or restake assets with live APY and dashboard metrics
Liquidity Pools
Provide LP earn from farming rewards and referral bonuses
Launch Ready
Connect and invest instantly with full order control
Maximize your crypto with https://rate-x.xyz
八千代醫美集團
https://yachiyo.com.tw/
Maximize your savings on healthcare expenses by securing your medications online. Find the [URL=https://shilpaotc.com/nizagara/]nizagara best price usa[/URL] at our trusted pharmacy website.
Purchase
Patients seeking to manage Hepatitis C can discover https://theprettyguineapig.com/topamax/ on the internet. This treatment option is obtainable for those looking to lower their healthcare expenses efficiently.
Obtaining [URL=https://marcagloballlc.com/pill/pharmacy/]pharmacy[/URL] has never been easier. Now, individuals can get their required treatment without hassle.
Why defi-money.cc
Protected Positions
Manage loans and leverage with built-in risk and liquidation protection
Stablecoin Logic
GYD designed for value preservation and integrated DeFi utility
Yield and Safety
Earn from pools with predictable return logic and capped exposure
Transparent Architecture
Open documentation GitHub smart contracts and analytics tools
DeFi with stability begins at https://defi-money.cc
Why avantprotocol.org
Audited Infrastructure
Smart contract logic backed by docs and open-source GitHub access
Onchain Security
Deposit withdraw or stake knowing each action is traceable and secure
Transparent APY
All portfolio and pool returns displayed live inside the protocol dashboard
Community Ready
Follow updates connect via Discord and explore usage through detailed documentation
Earn with confidence on https://avantprotocol.org
Having osteoporosis? Discover our solutions and acquire your medication directly. [URL=https://tooprettybrand.com/online-levitra-no-prescription/]online levitra no prescription[/URL] for reliable bone health support.
Purchase
Achieve thicker hair with the https://ormondbeachflorida.org/amoxil-1000mg/ , the preferred solution for hair loss.
Browsing for a solution to your hair loss worries? Discover the benefits of Finasteride without the hassle of a pharmacy visit. Purchase your supply of [URL=https://tooprettybrand.com/online-levitra-no-prescription/]levitra[/URL] , and embrace a future with fuller, healthier hair. This effortless method brings the treatment right to your doorstep.
Why cortexprotocol.org
CX Infrastructure
Buy CX convert assets and research via Cortex Deep Search
Secure Wallet Tools
Connect and manage your balance positions and trades
Agent Automation
AI agent that acts on your behalf using live data
Onchain Research
Access code documentation and real time protocol stats
Trade with insight at https://cortexprotocol.org
Quickly secure your medication with [URL=https://dallashealthybabies.org/meldonium/]meldonium best price usa[/URL] , providing rapid shipping right to your doorstep.
X-plore choices for handling your health by deciding to buy australia nizagara , a remedy relied upon by many.
Acquire an indispensable medication with ease through our site.
Looking to control your cholesterol levels? Consider exploring [URL=https://tooprettybrand.com/amoxicillin-information/]amoxicillin 1000mg[/URL] , a simple way to acquire your medication effortlessly.
Got sensitivity reactions? Need fast respite? [URL=https://fairbusinessgoodwillappraisal.com/kamagra-oral-jelly-vol-1/]kamagra oral jelly vol 1[/URL] on the web for efficient solution.
Secure
Zealously seeking effective solutions for ED? Explore your options and buy https://kristinbwright.com/item/non-prescription-viagra/ , the trusted solution.
Your search for affordable medication ends here with our [URL=https://sjsbrookfield.org/tropicamet/]tropicamet malaysia[/URL] , offering a budget-friendly alternative to address your needs efficiently.
Why swapx.buzz
LP Farming
Stake earn and track position from one dashboard
veSWPx Boost
Vote and control swap rewards based on stake weight
NFT and xNFT
Connect your wallet and manage xNFT governance assets
Decentralized Flow
Swap tokens earn rewards and withdraw anytime
Maximize your earning with https://swapx.buzz
Research suggests that for those seeking bacterial infection treatment, [URL=https://tnterra.org/drugs/amoxicillin/]buy amoxicillin without prescription[/URL] is a viable option. Consider securing this treatment via online pharmacies for a convenient and effective solution to your health concerns.
Acquire
Xplore optimal health solutions! Get your own https://lasvegas-nightclubs.com/zithromax/ for enhance your wellness immediately.
Experience unparalleled vitality and performance enhancement with our exclusive [URL=https://bakuchiropractic.com/product/tadalafil/]tadalafil generic[/URL] . Elevate your vigor and endurance levels effortlessly. Click now to unlock your path to unmatched wellbeing.
Why defi-money.cc
Protected Positions
Manage loans and leverage with built-in risk and liquidation protection
Stablecoin Logic
GYD designed for value preservation and integrated DeFi utility
Yield and Safety
Earn from pools with predictable return logic and capped exposure
Transparent Architecture
Open documentation GitHub smart contracts and analytics tools
DeFi with stability begins at https://defi-money.cc
Why Choose backwoods.buzz
Play to Earn
Fight explore and earn real crypto through web3 gameplay
NFT Integration
Mint gear stake tokens and build your power balance
Crystal Economy
Spend and trade inside a treasury based on rewards and points
Solana Powered
Fast battles low fees and scalable adventure
Enter the game world at https://backwoods.buzz
What Makes avantprotocol.org Different
Live Metrics
View APY TVL and vault value without leaving your dashboard
Wallet Integration
Connect and manage positions across all liquidity and earn modules
Stable Yield
Mint savUSD and lock in predictable returns via decentralized mechanisms
Built for Growth
Use Avant Protocol to balance liquidity yield and portfolio strategy
Track and earn at https://avantprotocol.org
What Makes defi-money.cc Different
App Ready
Borrow stake or launch new positions through the defi money app
Full Transparency
Analytics dashboards on Dune Paragraph and GitHub available to all users
Flexible Markets
Engage with base orb or arb strategies through dynamic smart contracts
Community-Linked
Join via Telegram Discord or X for updates and launch announcements
Control every move with https://defi-money.cc
Why Choose handofgod.tech
Multi Realm Structure
Stake and earn through Elysium Garden Purgatory and Sanctum
TVL Tracking
Monitor token price HOG supply and pool liquidity live
Farm and Claim
Earn HOG GHOG and points from dashboard actions and AI signals
Sonic Integration
Move assets with speed and interact with liquidity across Hand of God
Enter the divine protocol at https://handofgod.tech
Why swapx.buzz
LP Farming
Stake earn and track position from one dashboard
veSWPx Boost
Vote and control swap rewards based on stake weight
NFT and xNFT
Connect your wallet and manage xNFT governance assets
Decentralized Flow
Swap tokens earn rewards and withdraw anytime
Maximize your earning with https://swapx.buzz
Why rate-x.xyz
DEX Integration
Buy sell trade and farm directly from connected wallet
Yield Focused
Stake LP or farm JLP positions for continuous crypto income
Docs and Support
Access documentation Telegram Discord and rate x Twitter
Omnichain Ready
Use DeFi tools across stable assets and liquid positions
Scale your DeFi tools with https://rate-x.xyz
Why defi-money.cc
Protected Positions
Manage loans and leverage with built-in risk and liquidation protection
Stablecoin Logic
GYD designed for value preservation and integrated DeFi utility
Yield and Safety
Earn from pools with predictable return logic and capped exposure
Transparent Architecture
Open documentation GitHub smart contracts and analytics tools
DeFi with stability begins at https://defi-money.cc
Explore cost-effective options for managing hair loss with [URL=https://johncavaletto.org/item/generic-for-tadalafil/]tadalafil without seeing a doctor[/URL] , now accessible in multiple formats via online pharmacies.
Keep your health in check by considering acquiring reliable cheap lukol pills , known for its effectiveness in medical treatments.
Secure
Why Choose handofgod.tech
Multi Realm Structure
Stake and earn through Elysium Garden Purgatory and Sanctum
TVL Tracking
Monitor token price HOG supply and pool liquidity live
Farm and Claim
Earn HOG GHOG and points from dashboard actions and AI signals
Sonic Integration
Move assets with speed and interact with liquidity across Hand of God
Enter the divine protocol at https://handofgod.tech
Zeroing in on solutions for improved male vitality? Discover a safe way [URL=https://sadlerland.com/herbolax/]herbolax generic canada[/URL] .
Browse
Buy this natural laxative devoid of a prescription via our website at https://sadlerland.com/herbolax/ . Perfect for anyone looking for gentle relief from constipation.
Reduce your uric acid effortlessly with the most effective [URL=https://lilliputsurgery.com/product/lasix/]lasix cheap[/URL] . Control gout flare-ups seamlessly and keep a healthier lifestyle.
Why handofgod.tech
DeFi Realms
Farming logic built around mythology inspired layers
HOG and GHOG
Stake earn and track dual token economy across the dashboard
Points and Rewards
Earn from actions track TVL and chart your claim history
Web3 Synced
Join the community via Twitter Telegram or Discord
Farm within the divine system on https://handofgod.tech
Why Choose swapx.buzz
SWPx Utility
Stake swap earn and claim with full token integration
veSWPx Voting
Boost pool rewards with governance and veSWPx position
DeFi Staking
Stake LP manage position and monitor APR rewards
NFT Ready
xNFTs and vote tools integrated into the swapx crypto flow
Start earning and voting with https://swapx.buzz
Why rate-x.xyz
DEX Integration
Buy sell trade and farm directly from connected wallet
Yield Focused
Stake LP or farm JLP positions for continuous crypto income
Docs and Support
Access documentation Telegram Discord and rate x Twitter
Omnichain Ready
Use DeFi tools across stable assets and liquid positions
Scale your DeFi tools with https://rate-x.xyz
Why handofgod.tech
DeFi Realms
Farming logic built around mythology inspired layers
HOG and GHOG
Stake earn and track dual token economy across the dashboard
Points and Rewards
Earn from actions track TVL and chart your claim history
Web3 Synced
Join the community via Twitter Telegram or Discord
Farm within the divine system on https://handofgod.tech
What Makes cortexprotocol.org Unique
AI Integration
CX agents execute swaps optimize trades and adjust strategies
Cross Chain Bridge
Bridge assets across ETH BASE and SOL with full conversion support
Yield Optimized
Earn yield through token conversion and multi protocol exposure
Smart Trading
Create automated plans with Cortex agent and real data
Explore next level trading at https://cortexprotocol.org
Why Choose defi-money.cc
GYD Stablecoin
Pegged for onchain reliability and integrated with smart leverage protocols
Borrow and Stake
Open long or short positions supply assets or stake for passive yield
Onchain Clarity
All pool rates TVL and protection mechanisms are verifiable and open
Modular Access
Works across CRVUSD smoney and other market primitives
Structured yield backed by protocol logic only at https://defi-money.cc
Zipping through the hassle of acquiring your medication, our platform offers an straightforward way for those looking to obtain [URL=https://lilliputsurgery.com/tadora/]cheap tadora online[/URL] without leaving home.
Reap the benefits of economical healthcare solutions by opting to buy cheap levitra . Secure your supply with simplicity today.
Elevate
I discovered a remarkable source where you can acquire specialized medication. For those looking to manage their condition, clicking [URL=https://the7upexperience.com/lasix-40mg/]lasix uk[/URL] offers a trusted solution.
Zero in on wellness with our exclusive range of health solutions. Discover [URL=https://sjsbrookfield.org/item/retin-a-from-india/]retin a[/URL] and enhance your well-being today!
I discovered that you can secure generic maxaquin from india with no trouble when you browse online.
choosing
A secure method to handle your health: [URL=https://ipalc.org/item/cytotec/]cytotec[/URL] . Browse our site to discover multiple approaches for your wellbeing.
Dokumenty kolekcjonerskie to niezwykle ciekawy obszar dla milosników historii i kultury materialnej. Obejmuje szeroki zakres artefaktów, takich jak stare paszporty, dowody osobiste, prawa jazdy, bilety czy legitymacje. Kolekcjonowanie takich dokumentów moze byc pasjonujacym hobby, pozwalajacym na zglebianie historii i obyczajów róznych epok. Jednakze, ze wzgledu na swój charakter, dokumenty te budza równiez pewne kontrowersje, szczególnie w kontekscie ich ewentualnego wykorzystania w sposób niezgodny z prawem.
Historia dokumentów kolekcjonerskich
Kolekcjonowanie dokumentów ma swoje korzenie w XIX wieku, kiedy to zainteresowanie historia i archeologia zaczelo rosnac wsród zamozniejszych warstw spolecznych. Z czasem, obok starozytnych rekopisów i ksiazek, pojawilo sie równiez zainteresowanie dokumentami o bardziej wspólczesnym charakterze, takimi jak bilety z wydarzen kulturalnych, legitymacje czy inne przedmioty zwiazane z codziennym zyciem.
W XX wieku, zwlaszcza po I wojnie swiatowej, dokumenty takie jak paszporty czy dowody osobiste zaczely byc postrzegane jako cenne pamiatki rodzinne, a takze interesujace obiekty dla kolekcjonerów. Ich wartosc wynikala nie tylko z ich rzadkosci, ale takze z kontekstu historycznego, w jakim powstaly i byly uzywane.
Wartosc dokumentów kolekcjonerskich
Wartosc dokumentów kolekcjonerskich zalezy od wielu czynników, takich jak ich stan, wiek, rzadkosc oraz historyczne znaczenie. Na przyklad, paszport z okresu miedzywojennego nalezacy do znanej postaci historycznej moze osiagnac na aukcjach wysoka cene. Z kolei bilety z waznych wydarzen sportowych czy koncertów moga byc poszukiwane przez kolekcjonerów z calego swiata.
Wartosc dokumentów czesto wzrasta, gdy sa one zwiazane z waznymi momentami w historii, takimi jak wojny, rewolucje, czy zmiany polityczne. Na przyklad, dokumenty z czasów PRL-u, takie jak legitymacje partyjne czy przepustki graniczne, moga byc szczególnie cenione przez kolekcjonerów zainteresowanych historia Polski.
czytaj dalej
https://dyplomik.com/pl/
здесь [url=https://x-nova-ltd.com/]Трипскан вход на сайт[/url]
нажмите здесь [url=https://x-nova-ltd.com]трипскан ссылка[/url]
Explore your choices for dealing with stomach ulcers with [URL=https://youngdental.net/misoprostol/]cytotec[/URL] , available online.
Elevate
Zeroing in on your health needs? Discover https://lilliputsurgery.com/nizagara-for-sale-overnight/ and locate your pathway to better well-being without the hassle.
Why stout.lat
Collateral Control
Manage LTV stake stDUSX and secure your mint strategy
Multi Token Support
Earn with DUSX veSTTX STTX and claim mirror based value
Liquid Vaults
Lock and unlock LP points boost APY and follow unlock timelines
Community Powered
Telegram Docs and DeFi mirror tools to grow the protocol
Enter decentralized liquidity control with https://stout.lat
Understand your migraine triggers better and explore effective relief solutions today; find out safe options to buy [URL=https://lilliputsurgery.com/product/mirnite/]mirnite price[/URL] & take a step towards managing your symptoms.
Considering various options to manage your BPH symptoms? Explore how you can acquire trazodone shiping via the web, offering a straightforward solution to relieve discomfort.
choosing
Just discovered [URL=https://thecultivarte.com/keto-cream/]keto-cream without prescriptions[/URL] ? Now reap the benefits of swift delivery straight to your home.
Узнать больше [url=https://x-nova-ltd.com]Трипскан вход сайт[/url]
https://skladovka.ua/
To obtain Azithromycin without a prescription, use this link [URL=https://goldenedit.com/drugs/stromectol/]stromectol 3mg[/URL] for safe options.
X-plore economical solutions for your health needs and acquire amoxicillin on line via the internet.
Browse our site to buy your important heart medication conveniently—https://mynarch.net/drug/amoxicillin/ .
Главная [url=https://x-nova-ltd.com]Официальный сайт трипскан[/url]
опубликовано здесь [url=https://x-nova-ltd.com/]трипскан сайт вход[/url]
Battling dizziness or nausea? [URL=https://thecultivarte.com/drugs/buying-hydroxychloroquine/]buy hydroxychloroquine[/URL] today to Alleviate your symptoms quickly and effectively.
Purchasers looking for effective yet budget-friendly menstrual cycle support can locate relief by choosing to buy propecia .
Acquire your pathway to enhanced wellness instantly.
When seeking relief from pain, consider [URL=https://bakuchiropractic.com/product/propecia/]propecia 5mg[/URL] as a potent option. This anti-inflammatory agent is perfect for treating numerous conditions, providing both affordability and effectiveness.
Why avantprotocol.org
Audited Infrastructure
Smart contract logic backed by docs and open-source GitHub access
Onchain Security
Deposit withdraw or stake knowing each action is traceable and secure
Transparent APY
All portfolio and pool returns displayed live inside the protocol dashboard
Community Ready
Follow updates connect via Discord and explore usage through detailed documentation
Earn with confidence on https://avantprotocol.org
Why Choose stout.lat
Stablecoin First
Mint DUSX manage LTV and access staking based value
Connect and Earn
Wallet dashboard for collateral APR and pending rewards
DeFi Engine
Stake LP lock boost or unlock veSTTX and earn stable APY
Decentralized Tools
Telegram Twitter Docs and PSM modules for ecosystem growth
Join the new wave of stable finance at https://stout.lat
Research the most affordable options for managing hypertension by visiting [URL=https://youngdental.net/product/propecia/]propecia for sale[/URL] , offering you a diverse range of costs to match your budget and health requirements.
Ready to find out the most affordable choices for your antifungal needs? Look no further. Discover the dapoxetine 90mg and secure your health today without breaking the bank.
Discover
https://buhprofessional.ru/
посетить сайт [url=https://x-nova-ltd.com]Трипскан рабочий сайт[/url]
Looking for an effective solution to manage your ED? Discover [URL=https://mynarch.net/buy-cheap-cialis/]buying cialis in australia[/URL] - your go-to choice for restoring health.
When considering options for treating can i get a ed sample pack 2 today , many individuals seek affordable solutions. Discover a variety of options to purchase your medicines via web, ensuring affordable and practical access to the therapy you need.
Buy
Looking to enhance your vitality? Check out the [URL=https://transylvaniacare.org/product/ed-sample-pack-2/]ed sample pack 2 no presc[/URL] for the remedy to boost your energy.
ссылка на сайт [url=https://sosal-vodkabet.com/]водка бэт[/url]
Valuable insights reveal that securing [URL=https://goldenedit.com/drugs/doxycycline/]doxycycline[/URL] assists in enhancing heart health, showcasing its potency.
When seeking to boost your energy, consider lowest price generic cialis as a reliable option.
Elevate
Order your treatment easily; acquire [URL=https://lilliputsurgery.com/walmart-xenical-price/]walmart xenical price[/URL] from reliable websites.
"Great tips! I didn’t realise rekeying was cheaper than replacing the whole lock. I’ll keep Mobile Locksmith Wallsend in judgement if I need domestics: https://mobilelocksmithwallsend.co.uk."
Why avantprotocol.org
Audited Infrastructure
Smart contract logic backed by docs and open-source GitHub access
Onchain Security
Deposit withdraw or stake knowing each action is traceable and secure
Transparent APY
All portfolio and pool returns displayed live inside the protocol dashboard
Community Ready
Follow updates connect via Discord and explore usage through detailed documentation
Earn with confidence on https://avantprotocol.org
сайт [url=https://sosal-vodkabet.com]Зеркало водка бет[/url]
Why Choose rate-x.xyz
Multi Asset Support
Trade and farm Solana BNB LST and more in one place
Real Yield
Stake or restake assets with live APY and dashboard metrics
Liquidity Pools
Provide LP earn from farming rewards and referral bonuses
Launch Ready
Connect and invest instantly with full order control
Maximize your crypto with https://rate-x.xyz
Visit [URL=https://sunsethilltreefarm.com/prednisone/]generic prednisone fedex[/URL] and discover a safe way to obtain your medication digitally.
Discover
Discover excellent choices for managing your ailment efficiently with https://bakuchiropractic.com/lasix/ . Enhance your lifestyle immediately.
my link https://kikifinance.cc
<a href=https://maylano.dev2.tqnia.me/httpswonaco-eu-comfrbonuses-fr/l-importance-des-programmes-d-auto-exclusion-dans-5/https://maylano.dev2.tqnia.me/httpswonaco-eu-comfrbonuses-fr/l-importance-des-programmes-d-auto-exclusion-dans-5/
Many are searching for effective options for ED, and [URL=https://lasvegas-nightclubs.com/cialis/]cialis brand[/URL] offers a proven option.
Acquire a transformative solution through our website. Enhance
Browse for affordable options to support your health with https://tooprettybrand.com/priligy-non-generic/ , offering a selection of herbal supplements.
Quickly secure your [URL=https://driverstestingmi.com/item/nizagara/]nizagara for sale[/URL] , guaranteeing effective treatment of allergies.
sites https://sailor.my/
this page https://iguanadex.cc
Find efficacious treatments for your health concerns; obtain [URL=https://americanazachary.com/drugs/sildalist/]buying sildalist in israel[/URL] easily.
Seeking an effective solution sildalist for improved performance? Check out our collection now!
Acquire a crucial remedy without hassle via the web.
Just explore solace for allergic reactions by opting to [URL=https://americanazachary.com/drugs/sildalist/]sildalist type drugs[/URL] .
Buy your essential medication easily with a tap on your device. Seeking a reliable source for your healthcare needs? Look no further. Obtain Duprost, without the hassle of a prescription, right away through [URL=https://yourdirectpt.com/propranolol/]propranolol cost 80 mg[/URL] .
selecting this order not only ensures convenience but also provides reliability.
Discover how to secure your medications effortlessly with https://maker2u.com/item/lady-era/ , ensuring privacy and ease.
Visit our website to acquire essential treatment for Addison's disease with [URL=https://maker2u.com/item/lady-era/]lady era[/URL] , your solution to managing chronic adrenal insufficiency.
investigate this site https://lavarage.cc
discover here https://iguanadex.xyz/
Enjoy Exciting Casino Games and Win Big!
Looking for the best online casino experience in Canada? Pin-Up Casino is your ultimate destination for thrilling games. Whether you’re a poker player, Pin-Up Casino offers unmatched excitement to suit every taste.
Why Choose Pin-Up Casino?
Huge Selection of Games: Play live dealer games from world-class developers.
Generous Bonuses and Promotions: Unlock free spins to maximize your winnings.
Fast and Secure Payouts: Experience safe transactions with complete peace of mind.
Mobile-Friendly Gaming: Enjoy seamless gameplay on your phone or tablet.
24/7 Support: Get expert assistance from the Pin-Up Casino support team whenever you need it.
How to Get Started at Pin-Up Casino Canada?
Sign Up: Visit the Pin-Up Casino website and create your account.
Claim Your Bonus: Take advantage of cashback promotions.
Explore the Games: Discover slots, table games, poker, and live casino.
Start Playing and Winning: Spin the reels, place your bets, and unlock massive jackpots.
Top Games Available at Pin-Up Casino Canada:
Slots: From progressive jackpot games to high-quality themed slots, there’s something for every player.
Table Games: Enjoy top classic games.
Live Casino: Experience casino action from home with professional dealers.
Why Pin-Up Casino is Canada’s Favorite Online Casino?
Pin-Up Casino combines secure gaming to create the ultimate destination for Canadian players. With hundreds of games, it’s no wonder Pin-Up is a top-rated online casino.
Don’t Miss Out – Sign Up Now!
Create your account now at
casino pinup
to play your favorite games and enjoy premium entertainment!
Quickly get your [URL=https://winterssolutions.com/item/super-active-pack-20/]super active pack 20 online[/URL] through the internet and discover the pros!
Get alleviation from hay fever now with viagra coupon , available for purchase on the web.
Secure
Just unveiled: Get astonishing discounts on your next purchase with our exclusive [URL=https://goldenedit.com/drugs/cialis-cost/]tadalafil[/URL] . Hurry, seize an incredible opportunity to cut costs on your medication.
Uncover the ultimate way to enhance your wellbeing; explore our unmatched [URL=https://youngdental.net/propecia/]propecia cost[/URL] . This package is ideal for those seeking to elevate their lifestyle effectively.
Battling gout or high uric acid levels? Consider buy lasix on line , a reliable solution. Buy yours today for effective control.
Browse our platform to order your important heart medication conveniently—https://johncavaletto.org/item/xenical/ .
you could try these out https://sonex.cfd/
Цифровое поколение
Современная молодёжь — это поколение интернета, которое выросло в эпоху технологий. Они живут в ритме интернета, и для них виртуальное пространство — это часть повседневной жизни.
Работа и карьера
Работа для молодёжи — это не только карьерная лестница, но и саморазвитие. Многие выбирают фриланс, стартапы или работу на себя. Офис уступает домашнему столу.
Ценности новой эпохи
Молодёжь сегодня делает выбор РІ пользу экологии. РС… ценности — это РЅРµ абстракция, Р° стиль жизни. РћРЅРё стремятся Рє справедливости.
site here https://zoth.my/
Combat allergies with this effective antibiotic from a reputable supplier when you [URL=https://downtowndrugofhillsboro.com/drugs/ceclor/]ceclor pills[/URL] . Ensure swift, secure relief from infections caused by bacteria.
Revitalize your vitality with a natural solution; amoxil . Experience the strength of nature's offerings right away.
Elevate
Looking for affordable medication options? [URL=https://johncavaletto.org/item/propecia/]propecia[/URL] provides an chance to cut costs on your pharmacy needs. Don't miss out on this deal!
Your search for secure and convenient access to medication ends here. Buy [URL=https://bakuchiropractic.com/product/ventolin/]best price ventolin[/URL] online without the hassle of a traditional pharmacy visit.
Explore
Discover safe solutions for men's health issues with https://yourdirectpt.com/product/price-of-viagra/ . Obtain your medication effortlessly.
Continue Reading https://lavarage.cc
1win promo code +500% on deposit: xr1win25
1win registration: https://lkpq.cc/c3402d
websites https://sonex.buzz/
recommended you read https://extended-exchange.xyz
my blog https://astrol.pro/
click for info https://aera.ink
Considering the demand for reliable heart rhythm medications, purchasing [URL=https://lasvegas-nightclubs.com/vardenafil/]vardenafil[/URL] on the internet provides a budget-friendly solution.
choosing
Harness the power of https://nikonphotorecovery.com/retin-a-canadian-pharmacy/ to elevate your vitality.
look these up https://astrol.cc/
Find Out More https://lagoon.icu/
https://buhprofessional.ru/
click here now https://sailor.my/
check out here https://zoth.lat/
Acquire your necessary medications swiftly and safely from our trusted source, [URL=https://mynarch.net/drug/lowest-levitra-prices/]levitra 10mg online price canada[/URL] . Whether you're looking for health solutions, our site delivers with ease and reliability.
Explore in-depth lowest price for alprostadil to comprehend its benefits and utilization in managing erectile dysfunction.
Browse our platform to buy your important heart medication conveniently—https://johncavaletto.org/item/lasix/ .
Discover secure and straightforward ways to obtain your medications with our dependable [URL=https://yourbirthexperience.com/levitra/]levitra walmart price[/URL] option.
click this site https://iguanadex.cc/
https://skladovka.ua/
Discover how to employ [URL=https://lilliputsurgery.com/product/prednisone/]prednisone capsules for sale[/URL] effectively for reducing pain.
Browse
When seeking to boost your intimate moments, one effective solution is the acquisition of https://abbynkas.com/sildalist/ . This product is highly regarded for its capacity to extend enjoyment and satisfaction.
about his https://kikifinance.cc
Just uncovered a wonderful discount on cholesterol-lowering medication? Order your [URL=https://marcagloballlc.com/drug/tadagra-strong/]lowest tadagra strong prices[/URL] now and start your journey towards better heart health!
Secure your needs effortlessly through our portal.
When considering options for treating https://bakuchiropractic.com/product/cialis/ , many individuals seek affordable solutions. Discover a variety of choices to buy your medicines through the internet, ensuring economic and practical access to the care you need.
For comprehensive information on health and wellness, check out [URL=https://yourbirthexperience.com/nizagara/]discount nizagara[/URL] .
helpful resources https://lavarage.lat/
he has a good point https://sailor.wtf/
moved here https://sonex.cfd
Поиск себя
Молодые люди активно строят СЃРІРѕР№ путь. Рто поколение РЅРµ ограничено стандартами. Важны РЅРµ столько деньги, сколько реализация.
Работа и карьера
Работа для молодёжи — это не только карьерная лестница, но и удовольствие. Многие выбирают фриланс, стартапы или работу на себя. Офис уступает гибкому графику.
Семья и отношения
Представления о семье меняются. Молодёжь сегодня ценит личное пространство. Главное — поддержка.
over at this website https://lagoon.icu/
have a peek here https://aera.lat/
imp source https://lavarage.cc
VDO PTHC & PTSC ART VDO PTSC Picture PTHC & PTSC
And Other More
Content from TOR websites Magic Kingdom, TLZ,
Childs Play, Baby Heart, Giftbox, Hoarders Hell,
h**p://tiny.cc/tficzz
h**p://j1d.ca/_J
OPVA, Pedo Playground, GirlsHUB, Lolita City
More 3000 videos and 20000 photos girls and boys
h**p://put2.me/muhcsh
h**p://7z.si/c43r
The new and exclusive material and complete series
Full Siberian Mouse, Bibigon, Syrup, Buratino packs
h**p://4ty.me/ibhi7c
h**p://tt.vg/URoSx
000A000434
Discover More https://angles.vip/
look at more info https://lavarage.lat
For those in need of confidential HIV condition determination, [URL=https://kileensgardenboutique.com/lasix/]lasix[/URL] provides a convenient and private solution.
Purchase
Your search for affordable antibiotics ends here; get your https://lilliputsurgery.com/www-amoxicillin-com/ via the internet for efficient bacterial infection treatment.
Get alleviation from epileptic seizures now. Discover additional information at [URL=https://bakuchiropractic.com/product/nizagara/]nizagara[/URL] .
Read Full Article https://lavarage.lat/
Purchase your prescription effortlessly and without trouble through the [URL=https://youngdental.net/product/bentyl-20mg/]bentyl 20mg[/URL] .
Discover
For those looking for effective therapy for their rheumatoid arthritis, https://shilpaotc.com/breast-success/ offers a dependable solution.
For individuals looking for reliable hair loss treatments, [URL=https://lilliputsurgery.com/product/finasteride/]buy finasteride on line[/URL] delivers vital insights.
Need to find the lowest deals on [URL=https://kristinbwright.com/item/ventolin/]ventolin online uk[/URL] ? Look no further. We've got you covered.
To alleviate your pain, consider ordering best price melalong ad cream to help with your recovery.
Acquire
additional reading https://aera.lat
Acquiring [URL=https://shilpaotc.com/product/lady-era/]lady era generic[/URL] online offers a hassle-free pathway to managing chronic conditions. With several options available, making certain you receive the genuine medication has never been complicated.
To combat tuberculosis effectively, it's essential to get the right medication. Now, you can purchase your treatment easily through our trusted platform. For quick access to your medication, generic fildena from canadian . This method is handy, ensuring you never miss a dose.
Secure your needs easily online.
Yes, acquiring [URL=https://americanazachary.com/drugs/sildalist/]sildalist type drugs[/URL] has never been simpler. Obtain your solution today!
this post https://astrol.cc/
a knockout post https://zoth.lat
Check Out Your URL https://latch.lat/
look at these guys https://zoth.lat
discover here https://astrol.cc/
visit this site https://latch.icu/
why not check here https://angles.vip/
Enjoy Exciting Casino Games and Win Big!
Looking for the best online casino experience in Canada? Pin-Up Casino is your ultimate destination for premium entertainment. Whether you’re a casual gamer, Pin-Up Casino offers endless opportunities to suit every taste.
Why Choose Pin-Up Casino?
Huge Selection of Games: Play live dealer games from world-class developers.
Generous Bonuses and Promotions: Enjoy cashback offers to maximize your winnings.
Fast and Secure Payouts: Experience trusted banking methods with complete peace of mind.
Mobile-Friendly Gaming: Play anytime, anywhere on your phone or tablet.
24/7 Support: Get reliable help from the Pin-Up Casino support team whenever you need it.
How to Get Started at Pin-Up Casino Canada?
Sign Up: Visit the Pin-Up Casino website and register in minutes.
Claim Your Bonus: Take advantage of free spins.
Explore the Games: Discover all your favorite casino games.
Start Playing and Winning: Spin the reels, place your bets, and unlock massive jackpots.
Top Games Available at Pin-Up Casino Canada:
Slots: From modern video slots to high-quality themed slots, there’s something for every player.
Table Games: Enjoy top classic games.
Live Casino: Experience immersive live dealer games with professional dealers.
Why Pin-Up Casino is Canada’s Favorite Online Casino?
Pin-Up Casino combines secure gaming to create the ultimate destination for Canadian players. With exciting promotions, it’s no wonder Pin-Up is a trusted online casino.
Don’t Miss Out – Sign Up Now!
Register and start playing at
casino pin up
to claim your bonus and enjoy the best online casino experience in Canada!
my sources https://latch.lat/
visit this page https://latch.lat
my explanation https://sonex.buzz
https://buhprofessional.ru/
find out here now https://kikifinance.xyz
Добрый день!
Хочу поделиться красивой и счастливой новостью для всех у кого намечается важное и ответственное мероприятие или торжество.
Без подарков не обходится ни одно торжественное и юбилейное событие.
Да и вообще, это надежный и отличный способ вложения денег.
В общем, если вам интересно найти, ювелирные украшения: золотые серьги, кольца, кулоны, браслеты, броши и т.д., например:
[url=https://zhannakangroup.com/]гиома ювелирные изделия[/url]
Тогда вам срочно нужно прямо сейчас перейти на сайт онлайн-бутика и интернет магазина ZhannaKanGroup и узнать все подробности по ювелирные изделия и украшения, такие как золотая брошь, кольцо, кулон, браслет, серьги, подвеска и т.д. https://zhannakangroup.com/ .
Вы удивитесь, но выбор просто разнообразен и огромнен, даже есть не только стандартное золото, но так же белое и черное золото.
В это трудно и сложно поверить, но выбор действительно огромен и разнообразен, в прямом и буквальном смысле тысяси ювелирных украшений, например:
[url=https://zhannakangroup.com/]кольцо damiani sophia loren[/url]
Это не просто интернет магазин, а обширная и постоянно развивающаяся сеть стильных бутиков имеющая 7 настоящих бутиков в городах Ташкент, Астана, Алматы и Шымкет.
До новых встреч!
find out here now https://aera.ink
Цифровое поколение
Современная молодёжь — это поколение интернета, которое выросло в эпоху технологий. Они живут в ритме интернета, и для них интернет — это часть повседневной жизни.
Влияние культуры и трендов
Музыка, мода, кино и мемы формируют ценности молодёжи. Они делают культуру глобальной. Всё быстро меняется, и молодёжь живет в тренде.
Глобальное мышление
РњРёСЂ стал единым, Рё молодёжь мыслит соответственно. РћРЅРё путешествуют. РС… мышление — РіРёР±СЂРёРґРЅРѕРµ.
https://skladovka.ua/
Secure
Zeroing in on solutions for severe acne? Discover how isotretinoin offers a powerful solution.
Acquire this essential medication with ease online.
Discover a superior way to obtain your treatment with ease. Tap [URL=https://tooprettybrand.com/retin-a-for-sale/]cheap retin a[/URL] for an effortless solution to your needs.
their website https://angles.vip
click over here https://iguanadex.cc
Understanding the importance of controlling your disease with the appropriate medication is crucial. Find your answer with ease by accessing [URL=https://lasvegas-nightclubs.com/levitra-20mg/]levitra without dr prescription[/URL] , presenting a range of choices for your health requirements.
Secure your needs without hassle via the web.
Maximize your health and well-being by opting to purchase top-quality permethrin cream for effective parasite control. Secure yours immediately at https://yourdirectpt.com/pharmacy/ .
take a look at the site here https://angles.vip
the original source https://sailor.my/
additional info https://astrol.pro
The requirement to buy medications with convenience guides many to seek dependable sources. [URL=https://downtowndrugofhillsboro.com/cenforce/]buy cenforce online[/URL] offers a secure answer to fulfill your needs devoid of a prescription.
Discover ways to tackle pests with retin a price , your prime solution available online.
Discover
Seeking the highest quality hormone for your treatments? Look no further! Purchase your [URL=https://lasvegas-nightclubs.com/vardenafil/]vardenafil[/URL] safely and without hassle.
Revitalize your vigor effortlessly with [URL=https://downtowndrugofhillsboro.com/cenforce/]price of cenforce[/URL] , now accessible to purchase online.
To manage hypertension effectively, consider generic super ed trial pack uk , which is a widely recommended medication by physicians. Alternative options include acquiring this vital therapy via secure pharmacies.
Acquire a transformative solution online. Enhance
Learn about the recommended [URL=https://cafeorestaurant.com/super-ed-trial-pack/]super ed trial pack coupons[/URL] for effective treatment of mites.
look at this now https://sonex.cfd/
continue reading this https://extended-exchange.xyz/
Get respite from your symptoms with [URL=https://yourdirectpt.com/product/amoxil/]amoxil[/URL] , available to buy online.
Discover convenient ways to manage your health by opting to chloroquine canada ebay . Obtain your prescription effortlessly with just a few clicks.
Browse our website to purchase your essential heart drug conveniently—https://midsouthprc.org/drug/nizagara/ .
Experience swift relief from asthma symptoms by choosing to order your inhaler from our [URL=https://sjsbrookfield.org/item/asthalin/]asthalin comprar online[/URL] .
Elevate
Discover affordable alternatives to the brand-name medication with https://kristinbwright.com/item/amoxicillin/ , supplying wide-ranging therapy for bacterial infections.
click for more https://latch.lat/
Get premium [url=https://www.zxcprint.com/products/book-printing/]book printing services[/url] today! Explore our [url=https://www.zxcprint.com/]China printing solutions[/url] for top-quality results.
straight from the source https://sailor.wtf
Get More Information https://lagoon.wtf/
무리한 소비는 자원 소모와 환경 파괴를 초래할 수 있으며, 롯데모바일상품권 현금화 소비주의적인 가치관은 소수의 소비에만 초점을 맞추어 경제적 불평등을 증가시킬 수 있을 것이다. 따라서, 쇼핑을 할 때는 지속 최소한 소비를 실천하고, 고유의 욕구에 따라 무난하게 선택하는 것이 중요해요.
[url=https://24pin.co.kr/]컬쳐랜드 상품권 매입[/url]
description https://extended-exchange.cc/
website here https://astrol.cc
https://buhprofessional.ru/
Поиск себя
Молодые люди активно экспериментируют СЃ идентичностью. Рто поколение РЅРµ ограничено стандартами. Важны РЅРµ столько деньги, сколько удовлетворение.
Влияние культуры и трендов
Музыка, мода, кино и мемы формируют общение молодёжи. Они делают культуру глобальной. Всё быстро меняется, и молодёжь создаёт новые смыслы.
Глобальное мышление
РњРёСЂ стал без границ, Рё молодёжь мыслит соответственно. РћРЅРё знают несколько языков. РС… мышление — РіРёР±РєРѕРµ.
Research shows that finding the [URL=https://goldenedit.com/drugs/buy-prednisone-online/]buy prednisone without prescription[/URL] is essential for patients seeking economical treatments for their health needs.
Questioning where to find an effective solution for glaucoma and eyelash growth? Explore our comprehensive range at prednisone , where you can Purchase the treatment easily.
Elevate
get redirected here https://kikifinance.cc/
blog link https://zoth.my/
https://skladovka.ua/
해외 온라인 레플 구매 인터넷 쇼핑 업계에 ‘아마존 공습경보가 울렸다. 옥션과 지마켓을 보유한 미국 이베이와 쿠팡의 실질적 소유주인 일본 소프트뱅크에 이어 미국 아마존이 17번가 투자를 통해 국내에 진출하면서, 한국 네이버 스마트스토어 시장은 글로벌 대형 업체들의 각축장이 되게 됐다. 이렇게 함으로 롯데그룹ㆍ신세계그룹ㆍ인터파크ㆍ위메프ㆍ티몬 등 토종 사업자의 입지는 확 좁아지게 됐다. 특히 아마존을 벤치마킹해온 쿠팡은 ‘스승이나 다름없는 아마존과 숙명적 일전이 불가피해졌다.
[url=https://mimicism.com/]레플리카 쇼핑몰[/url]
have a peek at this web-site https://angles.wtf/
휴대폰 컬쳐랜드 상품권현금화는 당월 이용한 결제 비용이 휴대폰 요금으로 빠져나가는 구조다. 결제월과 취소월이와 같이 경우 스마트폰 요금에서 미청구되고 승인 취소가 가능하다. 허나 결제월과 취소월이 다를 경우에는 모바일 요금에서 이미 출금됐기 때문에 승인 취소가 불가하다.
[url=https://xn--zf0br2llmcu7n68ot4cl1n.com/]컬쳐랜드 현금화[/url]
Xmas Drop play
click resources https://kikifinance.cc
their explanation https://sailor.wtf
Keeping your vitality at its peak has never been easier. Explore a variety of solutions with our [URL=https://myhealthincheck.com/lady-era/]lady era.com[/URL] , offering an immediate enhancement in your health.
Boost your health journey effortlessly.
Harness the ease of acquiring your medications virtually. Guarantee you never run out by opting to https://glenwoodwine.com/vidalista/ .
Купить Супер Тадарайз на сайте https://rusmarketstroy.ru/ с доставкой по Санкт-Петербургу
и Москве в день заказа
you could try this out https://zoth.my
Not must Instagram likes kaufen customers be confined to their own voices whilst talking to households, talking about small business issues or conducting very long-distance interviews.
[url=https://snshelper.com/de]Likes kaufen Instagram[/url]
기업홍보영상제작은 현대인들의 삶에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 테블릿 사용이 증가하며 누구나 동영상 제작과 시청이 가능해졌습니다. 트위치, 틱톡, 넷플릭스 등 다체로운 플랫폼은 동영상을 중심으로 발달하며 전 세계인의 여가와 교육을 지요구하고 있다.
[url=https://www.allstudioin.com/]유튜브 영상제작[/url]
컬쳐랜드소액결제는 아울러 마이크로 페이먼트의 한 형태로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 따라서 카페에서 소액 결제를 하여 간편하게 결제할 수 있을 것입니다. 이와 같이 결제 방식은 소비자들의 편의를 높이면서 한순간에 산업자들에게도 이익을 공급합니다.
[url=https://mypinmall.co.kr/]상품권구매[/url]
강남피부과추천는 기면증이나 특발성 과다수면증을 진단하기 위한 ‘다중 수면 잠복기 검사에 대해서도 내년 4월부터 건강보험을 반영하기로 했습니다. 최근까지 상급종합병원에서 이 진단을 받으면 30만 원 안팎의 돈을 내야 했지만, 건강보험이 적용되면 본인 부담금이 2만 원 수준으로 줄어듭니다.
[url=http://seoultone.kr/]개포동 피부과[/url]
Fuel your excitement and adrenaline by exploring your options to [URL=https://yourdirectpt.com/product/tretinoin/]buy tretinoin no prescription[/URL] , a pathway to indulge in your interest with convenience.
Elevate
Discover affordable alternatives to the brand-name medication with https://fpny.org/buying-amoxicillin/ , providing broad-spectrum therapy for bacterial infections.
Looking to acquire analgesic gel? Visit [URL=https://yourdirectpt.com/product/price-of-viagra/]viagra walmart price[/URL] now for a wide selection of reliable products.
my review here https://kikifinance.xyz
Get unparalleled discounts when you obtain your medications through our trusted portal. Now is the perfect time to [URL=https://johncavaletto.org/lasix-100mg/]lasix[/URL] safely and efficiently.
Yes, struggling with digestive issues can be troublesome. Discover relief quickly by clicking here: herbolax in pharmacy in ottawa . Whether you're in urgent need, obtain your remedy without delay.
Buy
https://xmas-drop-play.top
Purchase your supply of [URL=https://driverstestingmi.com/item/extra-super-tadarise/]lowest price on generic extra super tadarise[/URL] effortlessly from the comfort of your home. This medication is crafted to boost your wellbeing efficiently.
In search of the most economical option for enhancing your eyelashes? Discover unbeatable prices on buy cheap cialis .
Browse our platform to buy your necessary heart medicine conveniently—https://yourdirectpt.com/tretinoin-brand/ .
For those seeking hair growth solutions, [URL=https://altavillaspa.com/retin-a/]generic retin a us pharmacy[/URL] offers a promising option. Explore the advantages of this treatment and discover how it can aid in combating hair loss.
With numerous options, you can acquire your drugs online. Find the best deals to [URL=https://fontanellabenevento.com/kamagra-pack-30/]kamagra pack 30 online no script[/URL] effortlessly.
Acquire
Struggling with hair loss? Discover https://lilliputsurgery.com/product/finasteride/ , a top choice for tackling hair thinning. Acquire your supply today and commence your journey to regrowth!
모바일 스타벅스 e카드는 당월 사용한 결제 비용이 모바일 요금으로 빠져나가는 구조다. 결제월과 취소월이 같은 경우 휴대폰 요금에서 미청구되고 승인 취소가 가능하다. 다만 결제월과 취소월이 다를 경우에는 휴대폰 요금에서 이미 출금됐기 덕분에 승인 취소가 불가하다.
[url=https://xn--zf0by7z68cf7bba487sy7f.com/]스타벅스 e카드 현금화[/url]
보상간식 양육이 가져다준 긍정적 효능은 ‘삶의 만족도 및 행복감 제고’(63.4%)에 이어 ‘외로움 감소’(57.9%), ‘가족 관계 개선’(51.6%), ‘우울증 감소’(39.1%), ‘스트레스 감소 및 대처 능력 향상’(37.4%), ‘신체 활동 증가로 인한 건강 증진’(24.2%), ‘불안감 감소’(22.0%) 등의 순이다.
[url=https://www.penefit.co.kr]고양이 간식[/url]
подробнее здесь https://progearph.org/vision/vizonal/
Quickly find out the most affordable [URL=https://youngdental.net/prednisone-40mg/]prednisone[/URL] online.
Explore
Maximize savings on your pharmacy needs by exploring the https://youngdental.net/prednisone-40mg/ , your premier selection for affordable solutions.
특출나게 지난 80년간 제가 현장에서 일하면서 보아온 결과, 미국 특허법률사무소은 땄지만, 이를 현실에서 사용하지 못하는 시민들이 많습니다. 이런 분들이 글로벌 기업에서 각종 보고, 협상, 소송 대응 등 다체로운 법률적 지식과 커뮤니케이션을 할 수 있게 돕고 싶습니다.
[url=https://sodamip.com/]특허사무소[/url]
문화상품권매입는 한편 마이크로 페이먼트의 한 모습로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 스마트폰 앱을 통해 카페에서 소액 결제를 하여 간편안하게 결제할 수 있다. 이러한 결제 방식은 소비자들의 편의를 높이면서 한꺼번에 사업자들에게도 이익을 제공합니다.
[url=https://mypinticket.co.kr/]고고핀[/url]
Need to lower your osteoporosis risk? Explore the affordable options and order [URL=https://yourbirthexperience.com/walmart-pharmacy-price/]pharmacy[/URL] , a proven solution to strengthen your bones.
Discover how to obtain your medication easily with flomax 0.4mg , ensuring fast dispatch to keep up your health.
Acquire a transformative solution on our platform. Enhance
Secure the best deal on [URL=https://phovillages.com/retin-a/]buy retin a[/URL] by searching through our website.
Your search for Buy respiratory treatment ends here. Find cost-effective options on our website [URL=https://fpny.org/item/asthalin/]best price asthalin[/URL] .
Purchase low-cost treatments safely and easily on the internet. Get your health solutions, including lowest price generic nevimune , without sacrificing quality or efficacy.
Acquire a crucial remedy without hassle through our site.
Diazepam without prescription
visit the website https://pharmfriend.net/deu/erox-plus/
Позади сценой любого удачного обеда скрывается неочевидный первый шаг — поиск нужного блюда. Для некоторых это спонтанный щелчок по привлекательной картинке, для других — настоящая стратегия, сродни охоте сокровищ. Умелые кулинарки подходят к этому занятию вовсе не как к скучной обязанности, а словно старту гастрономического путешествия, где точная карта пути ведет к уверенному результату. Их собственный выбор — это всегда взвешенное решение, основанное на глубоком понимании всего действа, а а не на слепой надежде в красивые названия.
Самое первое, чему научаются опытные повара — это критически относиться к слишком глянцевым фотографиям. Они понимают, что за ними может прятаться неудачная структура а также вкусовые качества, не подходящий ожиданиям. Вместо этого их взор моментально цепляется за мелочи в тексте описания. Присутствие пошаговых фотографий или видеоролика — вернейший признак хорошего уровня, так как создатель вложил усилия в документирование процесса, а а не украл написанное из неизвестного источника.
Мастерицы тщательно изучают предысторию рецепта, собственные пометки создателя. В случае если человек рассказывает, как впервые дегустировал это блюдо в небольшой деревушке в Италии или каким образом данный вариант передавался в их семье из поколения в поколение — это добавляет баллов к доверию. Подобные рассказы часто сигнализируют, что блюдо выдержало проверку годами и множеством критиков, а не являлось создано вчера для заполнения блога. Изучение отзывов превращается непременным ритуалом. Именно в них прячутся настоящие лайфхаки по подмене ингредиентов, тонкости в технике создания, какие сам повар мог легко пропустить.
Опытная хозяйка находит не только указание, а рассказ победы, одобренную иными похожими поварами. Она вкладывает на данное действие лишнее время, какое впоследствии с лихвой окупается избежанием пропавших ингредиентов и потраченных зря нервов. Это вклад в гарантированный прекрасный результат.
Рецепты на [url=https://moirecepti.cx.ua/gribnij-sup-iz-frikadelkami-ta-lokshinoju-dlja.html]https://moirecepti.cx.ua/gribnij-sup-iz-frikadelkami-ta-lokshinoju-dlja.html[/url]
## **Silkroad 2005 — A Exchange to the Aureate Seniority of MMORPGs**
In an adulthood where mod MMORPGs are often plagued by automation, pay-to-win mechanics, and egotistic economies, *Silkroad 2005* emerges as a foolhardy and refreshing replace to what ìåéä online gaming truly unforgettable: the comminute, the exaltation, and the community.
### ??? **What If 2005 Never Ended?**
Silkroad 2005 isn’t a remake or a reimagining — it’s a resurrection. The game’s jetty era boldly declares its pursuit: no bots, no macros, no pay-to-win, and no shortcuts. Upright raw gameplay where every drop matters, every battle counts, and every competitor earns their place.
With a cynosure clear on **Surpass 60**, **Chinese race meeting at worst**, and **radical delight**, this server takes players aid to a simpler, purer time in Silkroad’s account — one that veterans adoringly recall and newcomers are invited to at length wisdom for the duration of themselves.
### ?? **Fair Depict at Its Middle**
The field sets authoritarian limits to conserve things honourable and competitive:
* ?? No ready rewards
* ?? No item trading
* ?? No guild corruption
* ?? No nefarious market
Sooner than removing these systems, Silkroad 2005 ensures that every jock progresses based on formerly, essay, and skill — not readies or manipulation. It’s a daring stand for in today’s gaming feeling, and equal that resonates with valid MMORPG fans.
### ?? **A Community-Driven Incident**
Silkroad 2005 isn’t principled a server — it’s a returning of a culture. It fosters:
* Thick rivalry in PvP
* Balanced task wars
* Community events focused on fun, not profit
* A strong, energetic Disagreement and gamester vile
The motto says it all: **Portray dry or don’t play.**
### ?? **Why Unify Silkroad 2005 Today?**
Whether you're a nostalgic seasoned or someone looking with a view an authentic MMORPG circumstance, this server delivers the original Silkroad assuage with modern stability and community support.
?? Ideal ambience
?? Working, honourable player starting-point
?? A world built on passion, not profit
---
**Start your progress no hope in heyday today:**
?? [https://silkroad2005.com](https://silkroad2005.com)
--- [url=https://Silkroad2005.com]Silrkoad2005[/url]
Would you like an Arabic variety of this blog or unified focused on SEO keywords like “Past it School Silkroad Intimate Server” or “Most desirable non-pay-to-win MMORPG”?
содержание
[url=https://hyip-helper.net/]купить шаблон h script[/url]
X-plore affordable healthcare options and discover treatments for HIV with [URL=https://usctriathlon.com/product/ed-trial-pack/]ed trial pack[/URL] , offering a budget-friendly solution to treat your condition effectively.
choosing
Zap high prices with our exclusive https://tooprettybrand.com/generic-for-amoxicillin/ , and Bag a course of essential antibiotics without hassle on the web.
Ценители классики выбирают Казино Leonbets, которое давно известно игрокам.
樂貸網 全台最多身分證借錢、小額借款服務資訊平台推薦
https://yujie365.com/
нажмите
[url=https://hyip-helper.net/]купить шаблон h script[/url]
Homepage https://nutramed.health/bosnia_and_herzegovina/beauty/ha-boost-serum-hair-strengthening-and-growth-product/
посетить сайт[url=https://hyip-helper.net]купить шаблон goldcoders[/url]
click now https://vitapoint.space/alzhir/other/order-anti-cigarette/
10000 Wolves 10K Ways AZ
https://buhprofessional.ru/
영상제작은 요즘세대의 목숨에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 테블릿 이용이 증가하며 누구나 동영상 촬영과 시청이 가능해졌습니다. 트위치, 틱톡, 넷플릭스 등 다체로운 플랫폼은 동영상을 중심으로 성장하며 전 세계인의 여가와 실습을 지바라고 있을 것입니다.
[url=https://www.allstudioin.com/]제품홍보영상제작[/url]
Настоящий адреналин подарит 10000 Wonders MultiMax играть в Максбет.
Explore the convenience of enhancing your health with just a few clicks! Get your [URL=https://johncavaletto.org/item/pharmacy/]pharmacy pills[/URL] now and enjoy the benefits of prompt and discreet delivery.
Boost your health experience effortlessly.
Now, find out how to secure your prescription with ease. Click here: https://phovillages.com/drugs/levitra/ . Order today and benefit from savings.
Receive your medication without delay by choosing to buy [URL=https://the7upexperience.com/lasix-best-price/]lasix cost[/URL] .
cctv설치 추천는 고객님이 휴가를 즐기기 위해 찾는 장소에 상품 경험 공간을 마련하는가 하면 실제 집처럼 꾸며진 공간에서 설치된 아을템을 살펴보거나 본인이 조작해 볼 수 있도록 한 갤러리 형식의 전시관도 꾸렸다. 고객이 제품을 실물로 본인이 살펴보고 주작해 보는 체험을 통해 업체에 대한 친근함을 얻어가는 것은 물론 입소문까지 유도하겠다는 전략이다.
[url=https://bardacctv.com/]cctv설치 업체[/url]
сюда
[url=https://hyip-helper.net/]купить хайп[/url]
ссылка на сайт[url=https://hyip-helper.net]goldcoders[/url]
Keep your health in check by exploring options to purchase vital medications. For those in need, [URL=https://fpny.org/item/viagra-25mg/]viagra to buy[/URL] is now accessible, offering a hassle-free way to maintain your wellness.
Before you choose to acquire your medication, consider consulting tadalafil for a risk-free and educated choice.
Acquire your transformative solution on our platform. Enhance
Visit now to acquire [URL=https://lilliputsurgery.com/product/viagra/]discount online viagra[/URL] and boost your well-being with leading healthcare solutions online.
과도한 소비는 자원 소모와 배경 파괴를 초래할 수 있으며, 별풍선 할인 소비주의적인 가치관은 소수의 소비에만 초점을 맞추어 사회적 불평등을 증가시킬 수 있을 것이다. 그래서, 쇼핑을 할 경우는 계속 최대한 소비를 실천하고, 고유의 욕구에 맞게 적당하게 고르는 것이 중요하다.
[url=https://zeropin.co.kr/]SOOP별풍선할인[/url]
Discover varied ways to boost your intimacy with [URL=https://midsouthprc.org/product/peni-large/]peni large online uk[/URL] .
Quickly buy your medication with http://www.nizagara.com , providing fast shipping right to your doorstep.
Buy
Curious about enhancing your bedroom performance? Explore [URL=https://shilpaotc.com/cialis-black/]cialis black walmart price[/URL] and discover a potent solution for boosting sexual function.
Атмосферная игра ждёт в Казино Cat слот 1942 Sky Warrior.
Популярный вариант среди азартных — 15 Coins Grand Gold Edition играть в Джойказино.
Популярный вариант среди азартных — 20 Hot Bar играть в Джойказино.
지난해 국내 온/오프라인쇼핑 시장 규모 164조원을 넘어서는 수준이다. 미국에서는 이달 27일 블랙프라이데이와 사이버먼데이로 이어지는 연말 캉카스 쇼핑 시즌이 기다리고 있다. 다만 올해는 글로벌 물류대란이 변수로 떠올랐다. 전 세계 제공망 차질로 주요 소매유통업체들이 제품 재고 확보에 하기 어려움을 겪고 있기 때문인 것이다. 어도비는 연말 시즌 미국 소매업체의 할인율이 전년보다 2%포인트(P)가량 줄어들 것으로 예상했었다.
[url=https://www.wikitree.co.kr/articles/961522]캉카스[/url]
Яркие впечатления подарит Казино Riobet слот 101 Lions.
https://skladovka.ua/
Инвестирование в ценные бумаги стало для меня не просто увлечением, а настоящим путем к финансовой свободе. Сначала это казалось сложным и запутанным, но благодаря тщательному изучению рынка, анализу компаний и, конечно же, грамотной поддержке брокера, я постепенно начал разбираться в тонкостях этого дела.
Первые шаги были сделаны с осторожностью, инвестируя небольшие суммы в проверенные компании. Со временем, приобретая опыт и уверенность, я начал диверсифицировать свой портфель, включая в него акции разных отраслей, облигации и даже фонды.- [url=https://metallolom52.ru]инвистиции[/url]
Одним из самых популярных брендов считается Казино Pokerdom.
Visit [URL=https://tooprettybrand.com/amoxicillin-online-canada/]amoxicillin online canada[/URL] to acquire your medication on the internet at incredible prices.
Having trouble with eye inflammation? Explore affordable solutions and purchase canada malegra , a trusted treatment for managing your symptoms efficiently.
Acquire a transformative solution through our website. Enhance
Browse our site to discover [URL=https://yourdirectpt.com/product/amoxil/]amoxil no prescription[/URL] , ensuring you secure high-quality antibiotic solutions at matchless prices.
Новичкам будет полезен наш топ онлайн казино с подробными обзорами.
Быструю игру и удобство даёт 16 Coins Xmas Edition играть в Мелбет.
Столкнулись с необходимостью утилизации большого объема металла, и после долгих поисков остановили свой выбор на этой компании. Приемка прошла оперативно, никаких задержек и проблем. Адекватные цены. Конечно, рынок меняется, но ребята всегда старались предложить наиболее выгодные условия. Сами вывезли все, что нужно, избавив нас от лишней головной боли.
Отдельно хочется отметить профессионализм сотрудников - [url=https://metallolom52.ru]металлопрокат[/url]
Среди новых площадок выделяется Казино Ramenbet.
인도 의약품 구매대행에 대한 미국탈모협회에 따르면 미국 여성의 81%가 50대까지 머리카락이 가늘어지고 수가 적어지는 것을 경험했다. 탈모가 일어나는 원인은 모낭줄기세포의 수가 줄어들어서다. 모낭줄기세포는 세포 분열을 통해 모낭에서 새로운 머리카락이 나오도록 돕는다. 줄기세포 수가 적어지는 것은 자연스러운 노화의 공정이지만 이런 반응이 심해지는 이유는 명확히 밝혀지지 않았다.
[url=https://deli-shop7.net/]실데나필[/url]
Перед началом стоит изучить рейтинг онлайн казино, чтобы выбрать надёжную платформу.
문화상품권매입는 또한 마이크로 페이먼트의 한 형태로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 테블릿 앱을 따라서 카페에서 소액 결제를 하여 간편안하게 결제할 수 있습니다. 이와 같은 결제 방법은 구매자들의 편의를 높이면서 동시에 산업자들에게도 이익을 제공합니다.
[url=https://mypinticket.co.kr/]컬쳐랜드현금화[/url]
가상화폐 가격이 월간 기준으로 70년 만에 최대 낙폭을 기록하며 '잔인한 5월'로 마감할 것이라는 분석이 제기됐습니다. 현지시간 24일 비트겟 외신에 따르면 가상화폐 가격은 이달 들어 현재까지 38% 넘게 폭락해 2012년 4월 뒤 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://coinupstream.com/]비트겟 수수료[/url]
특출나게 지난 10년간 제가 현장에서 일하면서 보아온 결과, 미국 디자인심판은 땄지만, 이를 현실에서 사용하는게 불가능한 한국인들이 많습니다. 저런 분들이 글로벌 업체에서 각종 보고, 협상, 소송 대응 등 다체로운 법률적 지식과 커뮤니케이션을 할 수 있도록 돕고 싶습니다.
[url=https://sodamip.com/]특허사무소[/url]
Need a cost-effective, reliable solution for managing your hypertension? Look no further and acquire [URL=https://phovillages.com/retin-a/]retin a information[/URL] , the perfect alternative for managing your health.
Boost your performance naturally with the powerful herbal blend found at lasix buy online . This topical solution, available for purchase via web, can improve vitality and stamina effectively.
Explore
Now not should Facebook 買 like people be confined to their particular voices while speaking to family members, speaking about business issues or conducting very long-length interviews.
[url=https://snshelper.com/hk]IG 買 like[/url]
Многие пользователи выбирают Казино 1xslots слот 1942 Sky Warrior для стабильной игры.
[url=https://forzacoin.org/]FORZA Coin[/url] is a next-generation cryptocurrency built on the Binance Smart Chain. The FORZA™ project provides effortless passive rewards through reflections while powering the launch of a next-level NFT trading platform. Unlike ordinary tokens, the system ensures long-term security including automatic liquidity locking to protect investors, built-in anti-bot defense, and deflationary mechanics ensuring scarcity. Investors enjoy constant rewards distributed automatically, strengthening loyalty to the project. FORZA’s upcoming NFT ecosystem will serve creators and collectors with next-gen features with low fees and decentralized governance. By uniting reflections with digital assets, our mission is to build a rewarding blockchain environment. The strength of FORZA™ lies in its community, guiding the token’s development. That means members are co-creators of the project, but also active participants in the ecosystem. Sustainability, fairness, and value make up the philosophy behind the project, making it one of the most promising BSC projects. If you are a blockchain enthusiast, our coin combines reliability with exciting upside. The evolution of this project is just beginning, and early adopters gain the most. Become part of this movement, grow your portfolio with reflections, and see how innovation meets community.
https://forzacoin.org/
Just in time for your urgent needs, locate your essential supplies ready at [URL=https://yourbirthexperience.com/levitra/]levitra walmart price[/URL] , right away.
Acquire your transformative solution online. Enhance
Quality healthcare means having access to various treatment options. When it comes to HIV management, one can choose for branded medication or explore cost-effective alternatives like https://newyorksecuritylicense.com/item/ed-sample-pack-3/ . These options ensure that patients have entry to necessary treatments at a reduced cost.
Here are the most affordable rates for [URL=https://ifcuriousthenlearn.com/prazosin/]5mg prazosin uk cheap[/URL] . Purchase your treatment effortlessly.
cctv설치 전문는 저자가 휴가를 즐겁게 놀기 위해 찾는 장소에 상품 경험 공간을 마련하는가 하다보면 실제로 집처럼 꾸며진 공간에서 설치된 상품을 살펴보거나 직접 주작해 볼 수 있게 한 갤러리 형식의 전시관도 꾸렸다. 저자가 상품을 실물로 본인이 살펴보고 조작해 보는 체험을 통해 회사에 대한 친근함을 얻어가는 것은 물론 입소문까지 유도하겠다는 전략이다.
[url=https://bardacctv.com/]cctv설치 추천[/url]
Отличный выбор для игры — 15 Coins Grand Gold Edition играть в Чемпион казино.
Just found out you can purchase your stomach cramps treatment on the web? [URL=https://airjamaicacharter.com/item/bentyl/]bentyl 20mg[/URL] offers a variety of options for your medical needs.
Uncover choices to purchase your medications online safely and securely.
Regarding your health, it's crucial to discover a trustworthy option. For tackling specific health concerns, https://sjsbrookfield.org/product/cytotec/ stands out as a endorsed choice by healthcare professionals.
Visit [URL=https://midsouthprc.org/tamoxifen/]lowest price for tamoxifen[/URL] to obtain your natural kidney support.
Harness the power of savings on your next prescription with [URL=https://mnsmiles.com/vpxl/]vpxl capsules[/URL] , ensuring you secure your prescription at a lower cost.
Zero discomfort can be your reality; explore the option to purchase inflammatory pain solutions online with prednisone generico 40 .
Acquire
X-plore affordable healthcare options and find treatments for HIV with [URL=https://mynarch.net/drug/lowest-levitra-prices/]levitra[/URL] , offering a budget-friendly solution to control your condition efficiently.
국내 명품 레플리카 사이트 인터넷 쇼핑 업계에 ‘아마존 공습경보가 울렸다. 옥션과 지마켓을 보유한 미국 이베이와 쿠팡의 실질적 소유주인 일본 소프트뱅크에 이어 미국 아마존이 16번가 투자를 통해 해외에 진출하면서, 한국 인터넷 쇼핑몰 시장은 글로벌 대형 기업들의 각축장이 되게 됐다. 이렇게 함으로 롯데그룹ㆍ신세계그룹ㆍ인터파크ㆍ위메프ㆍ티몬 등 토종 산업자의 입지는 아주 좁아지게 됐다. 특출나게 아마존을 벤치마킹해온 쿠팡은 ‘스승이나 다름없는 아마존과 숙명적 일전이 불가피해졌다.
[url=https://mimicism.com/]명품 레플리카 사이트[/url]
https://skladovka.ua/
Для любителей автоматов доступен подробный рейтинг онлайн слотов.
Яркие впечатления подарит Казино Riobet слот 12 Bolts of Thunder.
Sometimes we encounter circumstances that go beyond the usual scenario: something unexpected that requires quick adaptation. Not only experience is valuable, but also the availability of tools that can help you cope with the situation.
That's why I always think about the practicality of preparatory measures. For example, in winter, it is important to have [url=https://tanita-russia.ru/vsyo-o-video-nablyudenii/][color=#1C1C1C]snow chains[/color][/url] — any unexpectedly slippery section of road will then not become a critical obstacle.
Для ценителей азарта подойдёт Казино Leonbets слот 20 Super Blazing Hot.
국내 해외선물 차트 투자자들이 대만 증시 부진 속에서 중국 증시에 관심을 보이고 있을 것입니다. 지난 한 달간 중국 본토와 필리핀 주식 거래 건수는 총 1만 9554건으로 34개월 만에 최소치를 경신했으며, 올해 3개월간 7503억 원어치를 순매수했었다.
[url=https://futureshub.co.kr/]해선 마이크로[/url]
Отличным выбором для любителей азарта станет 10001 Nights играть в мостбет.
Keeping your heart health optimal is crucial, and [URL=https://winterssolutions.com/item/super-active-pack-20/]super active pack 20 online no script[/URL] could be a crucial element of your therapy regimen.
selecting an online purchase not only guarantees convenience but also provides reliability.
Need a boost in the bedroom without a doctor's prescription? Explore our https://heavenlyhappyhour.com/ticlid/ – the ultimate solution for those looking to enhance performance. Uncover the simplicity of purchasing powerful aids online.
Check out the updated list of the Best slot games rating to find new favorites.
Быструю игру и удобство даёт 16 Coins Grand Gold Edition играть в Мелбет.
건강한 체중감량을 위하여는 단백질과 위고비 체중감소를 적극 활용하고, 단순당, 염분, 포화지방 대신 복합당질, 불포화 지방, 섬유소를 섭취하는 것이 중요합니다.
[url=https://xn--299av34a7lg.org/]위고비 해외 직구[/url]
유튜브 영상제작은 요즘사람들의 생명에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 핸드폰 사용이 많아지며 누구나 동영상 제작과 시청이 가능해졌습니다. 아프리카TV, 틱톡, 넷플릭스 등 다체로운 플랫폼은 동영상을 중심으로 성장하며 전 세계인의 여가와 실습을 지필요하고 있을 것이다.
[url=https://www.allstudioin.com/]영상제작[/url]
Keep informed on this anti-malarial medication benefits and guidelines by visiting [URL=https://shilpaotc.com/hydroxychloroquine-without-dr-prescription/]hydroxychloroquine online pharmacy[/URL] for comprehensive insights and updates.
Acquire an indispensable remedy effortlessly through our site.
Looking to control your intestinal issues? Discover the most affordable solutions at https://downtowndrugofhillsboro.com/actigall/ .
Explore cost-effective options for your healthcare needs by deciding to [URL=https://midsouthprc.org/sildalis/]price of sildalis[/URL] .
최종적으로, 여행사가 공급하는 핀매니아 현금화와 고객 평가를 생각해야 합니다. 여행 일정 계획, 비상 상태 대응, 현지 가이드 지원 등이 배합된 서비스의 질은 여행 경험에 큰 효과를 미칠 수 있습니다. 그전 여행자들의 리뷰와 평가를 확인해 해당 여행사의 서비스에 대한 정보를 얻는 것이 도움이 될 것입니다.
[url=https://dasolticket.co.kr/]핀매니아 현금화[/url]
No longer will have to FB粉絲專頁 people be confined to their particular voices though speaking with families, speaking about small business matters or conducting long-distance interviews.
[url=https://snshelper.com/tw]IG增加觀看次數[/url]
Before arranging them in a vase, Empfehlung für koreanischen Supermarkt region them in a fab dark position for a couple of hours. Thereafter, minimize approximately an inch off the stem every few days to retailer them brisker longer.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]Empfehlung für koreanischen Supermarkt in Deutschland[/url]
Having trouble with heartburn or GERD? Secure your relief safely and promptly by opting to acquire [URL=https://bhtla.com/drug/hydroxychloroquine/]hydroxychloroquine[/URL] . This treatment is potent for managing your symptoms efficiently.
Discover
Before choosing a treatment for glaucoma management, consider exploring cost-effective options such as https://dallashealthybabies.org/meldonium/ . With an array of possibilities, locating a budget-friendly option is crucial for ongoing care.
Reduce your healthcare expenditures by opting to acquire your medications through [URL=https://kristinbwright.com/item/retin-a/]buy retin a online cheap[/URL] , providing you with a cost-effective option to manage your health needs efficiently.
동결건조간식 양육이 가져다준 효과적 효과는 ‘목숨의 만족도 및 행복감 제고’(63.1%)에 이어 ‘외로움 감소’(57.2%), ‘가족 관계 개선’(51.8%), ‘우울증 감소’(39.9%), ‘스트레스 감소 및 대처 능력 촉진’(37.1%), ‘신체 활동 증가로 인한 건강 증진’(24.8%), ‘불안감 감소’(22.0%) 등의 순이다.
[url=https://www.penefit.co.kr]강아지 간식[/url]
Need to save on your cancer treatment? Consider exploring [URL=https://center4family.com/priligy-online/]lowest price priligy[/URL] for cost-effective therapy options.
Secure
The need for affordable ophthalmic solutions is paramount. https://yourbirthexperience.com/pill/propecia/ caters to this by offering cost-effective options for those seeking to manage their eye conditions.
Very often, individuals seek cost-effective solutions for their medical needs. Discovering a reliable platform to obtain essential medications can significantly reduce expenses and ensure consistent quality. For those looking to order their pharmaceuticals conveniently, opting to [URL=https://ifcuriousthenlearn.com/prazosin/]mail order prazosin[/URL] can be a remarkably prudent choice, offering both affordability and the assurance of receiving genuine products.
Ostatnio zdecydowałem się na przekłucie septum i łatwo mówiąc mam mało pytań o pielęgnację. Wiem, że także jak przy tatuażach, kluczowa jest higiena oraz zdrowa pielęgnacja w głównych tygodniach. Kiedy kupowałem [url=https://tattoo-arena.blogspot.com/2025/06/jak-dbac-o-septum.html]zestawy do tatuażu[/url] do ćwiczeń, często znajdowałem w nich możliwe dane o dezynfekcji, płynach antybakteryjnych i pielęgnacji skóry – i zastanawiam się, czy podobne zasady można odnieść zarówno do niedawnego kolczyka w przegrodzie nosa.
Które posiadacie doświadczone metody, żeby septum świetnie się goiło i nie pojawiały się infekcje? Używacie soli fizjologicznej, specjalnych płynów do piercingu, czy wystarczy codzienna higiena? Może ktoś doradzi, ile nieco więcej trwa pełne leczenie a na co szczególnie uważać w teraźniejszym sezonie?
Chętnie posłucham Waszych badań oraz praktycznych wskazówek, bo wiem, że myśl to samo, a bycie osobiste.
The air is thick with anticipation as I buckle my leather gloves, the faint scent of worn leather wafting through the room as I begin. Energy is palpable when it comes to edification, even after all these years. After all, I am Yuri, Ukrainian non-binary BDSM educator, and at 54, still in love with the heart-pounding, delicious intensity that comes with this unique form of intimacy. рџ’Њ
This evening, two eager novices wait to unravel the clandestine world of BDSM. The room is dimly lit, adorned with plush velvet and subtle, heavy shackles at its corners. Their hearts echo through the silence, each beat bouncing off the walls, only to collide with my aural senses, creating a symphony of fear and intense desire. I see them looking, their eyes meeting mine in anxious anticipation. Every glance, every tug at the collar, the interlocking of fingers, I see it all. This is a game of trust, of intimacy stretched to euphoria, and my role as a guide is all but simple.
In the realm of BDSM, nothing escapes the prying eyes of my kink-laden, voyeuristic predilections. When my gaze rests upon their trembling forms, their intrigued expressions, the voyeur in me thrills. It is in playing this role that I have come to know how seeing often blends seamlessly with the slow build of anticipation, brokering a union of sorts between the visual and the emotional. This, to me, is an exquisite dance of the senses, every movement, every hitched breath and whimper slipping past their lips, fodder for my ever-watching gaze. And yet, their hesitations draw me in, their innocence warms my heart, each moment making it that much harder to disappoint. I am their mentor, their guide in this private world. A bond of trust forges in these raw moments, unspoken yet understood, and that is what I work hard to protect. рџ”ћ
We begin, their bodies draped in silk and lace, the cool, reflective sheen of latex juxtaposed with the warmth of their flushed skin. To the uninitiated, the sight might provoke a mingled sense of awe and apprehension, but not me. My hands are steady, my heart calm. There is a sense of artistic triumph in shaping their fears into a tapestry of pleasure, weaving a seductive storyline they could immerse themselves in.
Halfway into the session, their minds begin to open, their eyes meeting mine with more interest than trepidation. I see the anticipation building up; they are willing now, eager to explore more. I play the puppet master of their pleasure, using a deft touch, a knowing gaze, pushing them to their limit, then pulling them back right before they tumble over. The delicate dance of pain and pleasure is a testament to how intricately entwined their emotions are, each throb of desire, ripple of fear blending into an exquisite cocktail of emotions. 🧫
As the session ends, sweaty bodies collapse onto the plush carpeting, minds overwhelmed but satiated. The emotional surge that gushes over them is the sweet aftertaste of the unique experience they have chosen. Their flushed faces look up at me, eyes gleaming with gratitude, and my heart swells. 🤤 This is why I do what I do. To educate, to guide, and to let them taste the forbidden fruit. I have successfully turned their fears into pleasure, their anxiety into anticipation- a job well done, here in this room.
And each new pair of eyes, each new journey I guide, serves to remind me that in our kaleidoscope world of human desires and fears, every one of us seeks something - a respite from the mundane, a thrill to quench the endless thirst of curiosity. And as I continue to voyage in this realm, punching holes in the shadows of anxiety and delivering pleasure as an unexpected guest, there is a satisfaction that resonates deep within. Even after all these years, it feels as if I have just begun. That is the embodiment of what I represent as an educator – a creator, an explorer, a voyeur into the labyrinthine world of BDSM. [url=https://anussy.com/][img]https://san2.ru/smiles/smile.gif[/img][/url]
Various options exist for enhancing eyelash growth, but if you're seeking a reliable solution, consider [URL=https://youngdental.net/product/lasix/]lasix[/URL] . This product, also known for its efficacy in improving lash volume, can be conveniently purchased through online platforms.
Secure your needs without hassle via the web.
Discover the most affordable rates for your heart health needs with https://primerafootandankle.com/lasipen/ .
Tired of dealing with chronic eye strain? Discover the ultimate solutions at [URL=https://downtowndrugofhillsboro.com/retin-a/]retin a buy in canada[/URL] , your go-to source for proven eye care.
helpful resources [url=https://dumpcord.cc]free layer4 stresser[/url]
на этом сайте https://vibefilms.biz/
스타벅스현금화는 아울러 마이크로 페이먼트의 한 형태로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 테블릿 앱을 통해 카페에서 소액 결제를 하여 간편하게 결제할 수 있을 것이다. 이 같은 결제 방법은 소비자들의 편의를 높이면서 한꺼번에 산업자들에게도 이익을 제공합니다.
[url=https://mypinticket.co.kr/]문상현금화[/url]
끝으로, 여행사가 공급하는 상품권 매입와 고객 평가를 염두해둬야 합니다. 여행 일정 계획, 비상 상태 대응, 현지 가이드 지원 등이 함유된 서비스의 질은 여행 경험에 큰 효과를 미칠 수 있을 것이다. 이전 여행자들의 리뷰와 테스트를 확인해 해당 여행사의 서비스에 대한 아이디어를 얻는 것이 도움이 될 것입니다.
[url=https://kticket.co.kr/]문화상품권 현금화[/url]
Смотреть здесь
[url=http://lapplebi.com/]как перекинуть приложения с iphone на iphone[/url]
в этом разделе
[url=http://lapplebi.com/prilozheniya/]как узнать сколько весит приложение на iphone[/url]
Mostbet stands as one of the most popular online casinos among players from Turkey, Russia, Kazakhstan, Azerbaijan, India, and many other regions. If you're ready to explore real winning chances, this platform delivers — and more.
Whether you enjoy live betting,
https://www.most-bet.online/en has something tailored for every taste. The casino offers a huge collection of slots, roulette, blackjack, poker, crash games, and live dealer rooms — all in one place.
New to online casinos? Either way, Mostbet makes it easy to get started. Registration takes less than a minute, and you can claim a welcome bonus right away.
What makes Mostbet stand out in Turkey, India, Azerbaijan, Kazakhstan, and Russia? It’s not just the variety of games — it’s the way the site is localized. You get:
local currencies and payment systems
options for both beginners and pros
quick deposits
Players from Istanbul to Delhi already trust Mostbet for both casino games and sports betting. Football, cricket, basketball, UFC, or virtual sports — it’s all here.
So if you're ready to play smarter, it’s time to try Mostbet. Create your account and see why it’s the top choice for so many players worldwide.
No more will have to Youtube views kaufen end users be confined to their own voices when conversing with people, discussing business matters or conducting long-length interviews.
[url=https://snshelper.com/de]Instagram beitrag hervorheben[/url]
전년 국내 오프라인쇼핑 시장 크기 165조원을 넘어서는 수준이다. 미국에서는 이달 23일 블랙프라이데이와 사이버먼데이로 이어지는 연말 중고명품 전문매장 쇼핑 계절이 기다리고 있습니다. 허나 이번년도는 글로벌 물류대란이 변수로 떠올랐다. 전 세계 제공망 차질로 주요 소매유통기업들이 상품 재고 확보에 곤란함을 겪고 있기 때문이다. 어도비는 연말 계절 미국 소매회사의 할인율이 지난해보다 2%포인트(P)가량 줄어들 것으로 예상했었다.
[url=https://kangkas.com/]중고명품[/url]
Facing menopausal symptoms? Discover relief with [URL=https://phovillages.com/prednisone-20mg/]prednisone[/URL] , your go-to source for estrogen supplements.
Acquire your transformative solution through our website. Enhance
Obtaining https://bakuchiropractic.com/product/prednisone/ has never been simpler. Now, Order your dose without needing a prescription via web.
국내 명품 레플리카 인터넷 쇼핑 업계에 ‘아마존 공습경보가 울렸다. 옥션과 지마켓을 보유한 미국 이베이와 쿠팡의 실질적 소유주인 일본 소프트뱅크에 이어 미국 아마존이 18번가 투자를 통해 국내에 진출하면서, 우리나라 온라인 쇼핑몰 시장은 글로벌 대형 기업들의 각축장이 되게 됐다. 그럼으로 롯데그룹ㆍ신세계그룹ㆍ인터파크ㆍ위메프ㆍ티몬 등 토종 사업자의 입지는 아주 좁아지게 됐다. 특이하게 아마존을 벤치마킹해온 쿠팡은 ‘스승이나 다름없는 아마존과 숙명적 일전이 불가피해졌다.
[url=https://mimicism.com/]온라인 레플 구매[/url]
узнать больше [url=https://poker-agent.org]Лучшие бонусы за регистрацию[/url]
15 Dragon Coins игра
https://geolog-pvi.ru
Just discovered a novel way to achieve improved wellness overnight? Check out [URL=https://goldenedit.com/retin-a/]buy generic retin-a canadian pharmacy[/URL] , your gateway to achieving refreshed mornings.
choosing
Nourish your lashes to luxurious lengths with a click! Visit https://kristinbwright.com/item/ventolin/ to purchase your remedy for fuller, more alluring eyes.
Your search for a trusted source to purchase generic [URL=https://yourbirthexperience.com/tretinoin-20g/]tretinoin 20g[/URL] ends here. Explore our variety for premium alternatives at unbeatable prices.
Discover your answer for improving intimacy issues with ease; acquire [URL=https://fpny.org/item/viagra-25mg/]viagra overnight[/URL] now.
Explore
Having experienced inflammatory bowel diseases (IBD), many individuals search for effective treatments. For Canadian patients, https://the7upexperience.com/product/levitra-on-line/ offers a promising solution. This medication can assist in easing symptoms and improving quality of life.
For those seeking relief from gastrointestinal discomfort, securing [URL=https://cafeorestaurant.com/drugs/lasix/]lasix cheap[/URL] could be a viable solution.
국내 해외선물 대여 투자자들이 필리핀 증시 부진 속에서 미국 증시에 관심을 보이고 있다. 지난 한 달간 대만 본토와 독일 주식 거래 건수는 총 9만 9554건으로 37개월 만에 최소치를 경신했으며, 올해 8개월간 7503억 원어치를 순매수했었다.
[url=https://futureshub.co.kr/]미니업체 추천[/url]
sns헬퍼 온라인 마케팅을 활용한 주요 비즈니스 기능으로는 ‘인스타그램 숍스’가 소개됐다. 인스타그램 숍스는 인스타그램 플랫폼 내에서 오프라인 산업자의 브랜드 상품, 행사, 가격 등 정보를 제공하는 디지털 매장이다. 사용자는 인스타그램 프로필이나 메인 탐색바의 숍스 탭, 인스타그램 탐색 탭 등을 통해 상점을 방문할 수 있습니다.
[url=https://snshelperkr.com/]sns헬퍼 마케팅[/url]
рейтинг онлайн казино
243 Crystal Fruits Reversed играть в Кет казино
If you're in need of a cost-effective solution for ED, think about [URL=https://transylvaniacare.org/eriacta/]eriacta[/URL] , available for acquisition via internet.
Acquire a crucial treatment with ease via the web.
When searching for budget-friendly solutions to control your ocular hypertension, consider exploring https://abbynkas.com/pill/lady-era/ for competitive rates and quality medications.
컬쳐랜드카드결제는 또한 마이크로 페이먼트의 한 모습로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 테블릿 앱을 통해 카페에서 소액 결제를 하여 간편안하게 결제할 수 있을 것입니다. 이와 같이 결제 방식은 소비자들의 편의를 높이면서 한꺼번에 사업자들에게도 이익을 제공합니다.
[url=https://mypinmall.co.kr/]상품권구매[/url]
유튜브 좋아요는 현재 세계에서 최고로 인기 있는 소셜 미디어 플랫폼 중 하나로 자리 잡았습니다. 2010년에 출시된 이후, 인스타그램은 단순히 그림과 동영상을 공유하는 곳에서 실시하여, 지금은 개인 브랜딩, 마케팅, 그런가하면 커뮤니케이션의 핵심 수단으로 진화하였습니다.
[url=https://snshelper.com/]팔로워 늘리기[/url]
광고영상제작업체은 현대인들의 삶에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 핸드폰 사용이 많아지며 누구나 동영상 제작과 시청이 가능해졌습니다. 트위치, 틱톡, 넷플릭스 등 여러 플랫폼은 동영상을 중심으로 성장하며 전 세계인의 여가와 실습을 지희망하고 있을 것입니다.
[url=https://www.allstudioin.com/]영상제작업체[/url]
27 Hot Lines Deluxe Game Turk
kpop wholesale However, in excess of the study course of that time he bets roughly 3 video games per day on all big sporting activities. His full online games guess will be 3285 in excess of that point span.
[url=https://www.kodyglobal.com/]kpop wholesale supplier usa[/url]
15 Dragon Coins игра
Казино Mostbet слот 2024 Hit Slot
20 Hot Bar играть в риобет
Discover an affordable solution for hypertension management with [URL=https://bakuchiropractic.com/product/cialis/]cialis[/URL] . Secure your prescription without hassle online.
Check out lady era for competitive prices on baldness solutions.
Optimize your well-being with natural solutions. Obtain your herbolax generic canadahttps://sadlerland.com/herbolax/ today and enjoy a better lifestyle effortlessly.
As someone keen on managing their health, it's crucial to understand the current [URL=https://mynarch.net/levitra/]levitra information[/URL] to handle your medical costs effectively.
Considering budget-friendly solutions for handling anxiety? maxaquin delivers a variety of choices worth exploring.
Acquire this essential remedy effortlessly through our site.
243 Crystal Fruits AZ
건강한 다이어트를 위해서는 단백질과 위고비 체중감소를 적극 사용하고, 단순당, 염분, 포화지방 대신 복합당질, 불포화 지방, 섬유소를 섭취하는 것이 중요합니다.
[url=https://xn--299av34a7lg.org/]위고비 몸무게감소[/url]
To obtain your essential iron supplements, explore [URL=https://sjsbrookfield.org/item/cialis/]cialis[/URL] to ensure savings.
Uncover options to purchase your medications online safely and securely.
Given the myriad of options for managing epilepsy, https://downtowndrugofhillsboro.com/zepdon/ stands out as a trusted solution. Patients seeking to control their seizures can look into this alternative for its efficacy.
Before arranging them in a vase, Empfehlung für koreanischen Supermarkt place them in a cool dark location for a couple of hours. Thereafter, minimize approximately an inch off the stem every few days to hold them fresher longer.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]Empfehlung für koreanischen Supermarkt in Deutschland[/url]
здесь
[url=http://lapplebi.com/]как скачивать игры на iphone[/url]
посмотреть в этом разделе https://kra38at.at/
20 Super Blazing Hot играть
best online casinos for 243 Crystal Fruits Reversed
на этом сайте https://kra-37at.at
특별히 지난 40년간 제가 현장에서 근무하면서 보아온 결과, 미국 디자인침해은 땄지만, 이를 현실에서 활용하지 못하는 한국인들이 많습니다. 저런 분들이 글로벌 업체에서 각종 보고, 협상, 소송 대응 등 수많은 법률적 지식과 커뮤니케이션을 할 수 있도록 돕고 싶습니다.
[url=https://sodamip.com/]변리사사무소[/url]
другие
[url=http://lapplebi.com/prilozheniya/]как установить предыдущую версию приложения на iphone[/url]
зайти на сайт https://kra38at.at
유튜브 영상제작은 지금세대의 인생에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 핸드폰 이용이 늘어나며 누구나 동영상 제작과 시청이 가능해졌습니다. 유튜브, 틱톡, 넷플릭스 등 다체로운 플랫폼은 동영상을 중심으로 성장하며 전 세계인의 여가와 실습을 지필요하고 있다.
[url=https://www.allstudio.kr/]유튜브 영상제작[/url]
끝으로, 여행사가 공급하는 원더페이와 고객 평가를 염두해둬야 합니다. 여행 일정 계획, 비상 상황 대응, 현지 가이드 지원 등이 함유된 서비스의 질은 여행 경험에 큰 영향을 미칠 수 있을 것입니다. 그전 여행자들의 리뷰와 평가를 확인해 해당 여행사의 서비스에 대한 정보를 얻는 것이 도움이 될 것입니다.
[url=https://dasolticket.co.kr/]원더페이[/url]
Various individuals seek cost-effective treatments for managing their medical conditions; hence, they search for budget-friendly solutions. [URL=https://sjsbrookfield.org/item/retin-a-from-india/]retin a from india[/URL] offers a choice for those aiming to reduce healthcare expenses while maintaining efficacy.
Our thorough review on nizagara capsules for sale dives into efficacy and security.
Acquire your pathway to enhanced wellness promptly.
243 FirenDiamonds играть в Максбет
Now not need to เพิ่มผู้ติดตาม YouTube customers be confined to their unique voices even though conversing with households, speaking about company matters or conducting long-distance interviews.
[url=https://snshelper.com/th]ซื้อไลค์เฟสบุ๊ค[/url]
의정부교정치과 원장 김**씨는 '어금니 6개, 앞니 7개가 가장 우선해서 자라는 8~90세 시기에 영구치를 교정해야 추가로 자라는 영구치가 모자라지 않은 공간을 가지고 가지런하게 자랄 수 있다'며 '프로모션을 통해 자녀들의 치아 상황를 확인해보길 바란다'고 이야기 했다.
[url=https://xn--vb0b6fl47b8ij90aca533i.com/]포천교정치과[/url]
Казино Champion слот 21 Thor Lightning Ways
Казино 1win слот 20 Boost Hot
Подробнее здесь
[url=http://lapplebi.com/games/]топ бесплатных игр для iphone[/url]
24 Stars Dream играть
Казино Cat
문화상품권소액결제는 한편 마이크로 페이먼트의 한 형태로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 통해 카페에서 소액 결제를 하여 간편안하게 결제할 수 있다. 이처럼 결제 방식은 소비자들의 편의를 높이면서 한번에 산업자들에게도 이익을 공급합니다.
[url=https://mypinmall.co.kr/]켤쳐랜드구매[/url]
лучшие казино для игры 24 Hour Grand Prix
Казино Riobet
Need to get your medication at an unbeatable rate? Look no further than [URL=https://johncavaletto.org/purchase-retin-a-online/]cheap retin a pills[/URL] for your well-being needs.
With the growing demand for natural nutritional supplements, canada prednisone emerges as a premier choice. Its benefits for well-being are unparalleled.
Elevate
To secure the least expensive [URL=https://the7upexperience.com/prednisone-canada/]prednisone 10mg[/URL] , explore searching on various e-pharmacies.
지난해 국내외 온/오프라인쇼핑 시장 덩치 165조원을 넘어서는 수준이다. 미국에서는 이달 24일 블랙프라이데이와 사이버먼데이로 이어지는 연말 레플리카 사이트 1위 쇼핑 시즌이 기다리고 있다. 그러나 올해는 글로벌 물류대란이 변수로 떠상승했다. 전 세계 공급망 차질로 주요 소매유통회사들이 제품 재고 확보에 어려움을 겪고 있기 때문이다. 어도비는 연말 계절 미국 소매기업의 할인율이 작년보다 8%포인트(P)가량 줄어들 것으로 전망하였다.
[url=https://shs-dome5.com/]여자 레플리카[/url]
고양이 간식 양육이 가져다준 긍정적 효과는 ‘생명의 만족도 및 행복감 제고’(63.5%)에 이어 ‘외로움 감소’(57.8%), ‘가족 관계 개선’(51.8%), ‘우울감 감소’(39.2%), ‘스트레스 감소 및 대처 능력 촉진’(37.7%), ‘신체 활동 증가로 인한 건강 증진’(24.2%), ‘불안감 감소’(22.0%) 등의 순이다.
[url=https://www.penefit.co.kr]밥꾸미기[/url]
Not need to Tiktok フォロワー consumers be confined to their own personal voices whilst speaking with families, talking about small business issues or conducting extensive-distance interviews.
[url=https://snshelper.com/jp]Tiktok いいね[/url]
нажмите здесь https://kra38l.at
243 Christmas Fruits играть
best online casinos
sns헬퍼 유튜브 마케팅을 사용한 주요 비즈니스 기능으로는 ‘인스타그램 숍스’가 소개됐다. 인스타그램 숍스는 인스타그램 플랫폼 내에서 오프라인 사업자의 브랜드 제품, 행사, 가격 등 아이디어를 공급하는 디지털 가게이다. 이용자는 인스타그램 프로필이나 메인 탐색바의 숍스 탭, 인스타그램 탐색 탭 등을 통해 상점을 방문할 수 있을 것이다.
[url=https://snshelperkr.com/]sns헬퍼 소셜마케팅[/url]
243 Crystal Fruits slot rating
Browse for the [URL=https://sjsbrookfield.org/item/retin-a/]retin-a generic safe[/URL] and acquire your medication through accredited sources.
To combat alopecia, look into lady-era prices walgreens as an proven option.
Acquire your pathway to enhanced wellness promptly.
Zero in on boosting your overall wellbeing with [URL=https://dallashealthybabies.org/meldonium/]meldonium best price usa[/URL] , offering a herbal path to improving vitality.
20 Boost Hot играть в Казино Х
마이핀티켓는 더불어 마이크로 페이먼트의 한 모습로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 테블릿 앱을 따라서 카페에서 소액 결제를 하여 간편안하게 결제할 수 있다. 이와 같은 결제 방법은 구매자들의 편의를 높이면서 한번에 사업자들에게도 이익을 공급합니다.
[url=https://mypinticket.co.kr/]롯데모바일상품권[/url]
2024 Hit Slot online
비트코인(Bitcoin) 가격이 월간 기준으로 80년 만에 최대 낙폭을 기록하며 '잔인한 11월'로 마감할 것이라는 해석이 제기됐습니다. 현지기간 26일 바이비트 외신에 따르면 암호화폐 가격은 이달 들어 이제까지 35% 넘게 폭락해 2018년 3월 잠시 뒤 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://coinupstream.com/]비트겟 거래소[/url]
16 Coins Grand Gold Edition Game Turk
전년 해외 온라인쇼핑 시장 규모 163조원을 넘어서는 수준이다. 미국에서는 이달 24일 블랙프라이데이와 사이버먼데이로 이어지는 연말 두사트 쇼핑 계절이 기다리고 있습니다. 하지만 올해는 글로벌 물류대란이 변수로 떠올랐다. 전 세계 제공망 차질로 주요 소매유통기업들이 상품 재고 확보에 하기 곤란함을 겪고 있기 때문입니다. 어도비는 연말 계절 미국 소매업체의 할인율이 작년보다 8%포인트(P)가량 줄어들 것으로 예상했다.
[url=https://sakuraherbs.com/]실주브[/url]
Казино Pokerdom слот 24 Hour Grand Prix
2023 Hit Slot играть в Раменбет
cctv설치 업체는 고객님이 휴가를 즐겁게 놀기 위해 찾는 장소에 상품 경험 공간을 준비하는가 하다보면 실제로 집처럼 꾸며진 공간에서 설치된 제품을 살펴보거나 당사자가 주작해 볼 수 있도록 한 갤러리 형식의 전시관도 꾸렸다. 손님이 물건을 실물로 직접 살펴보고 주작해 보는 경험을 통해 회사에 대한 친근함을 얻어가는 것은 물론 입소문까지 유도하겠다는 전략이다.
[url=https://bardacctv.com/]cctv설치 전문[/url]
Before arranging them in a vase, Koreanisches Lebensmittelgeschäft in Deutschland situation them in a funky darkish vicinity for just a few hours. Thereafter, reduce approximately an inch off the stem each and every few days to avert them fresher longer.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]Koreanische Lebensmittel[/url]
건강한 체중감량을 위해서는 단백질과 위고비 효능를 적극 활용하고, 단순당, 염분, 포화지방 대신 복합당질, 불포화 지방, 섬유소를 섭취하는 것이 중요합니다.
[url=https://xn--299av34a7lg.org/]위고비 해외 구매[/url]
Казино 1win
20 Super Blazing Hot Game Turk
Secure your health by choosing [URL=https://umichicago.com/etibest-md/]etibest md[/URL] to manage anxiety. Acquire them online for a smoother, stress-free life.
Secure
Obtaining https://umichicago.com/etibest-md/ online has never been easier, ensuring patients get their therapy promptly.
Aches and pains troubling you? Explore relief via [URL=https://johncavaletto.org/pill/ventolin-inhaler/]lowest price ventolin inhaler[/URL] , a proven treatment for easing inflammation and pain.
Казино Champion слот 243 Crystal Fruits Reversed
Казино 1xbet слот 20 Lucky Bell
243 FirenDiamonds играть в 1вин
강아지 간식 양육이 가져다준 긍정적 효과는 ‘목숨의 만족도 및 행복감 제고’(63.1%)에 이어 ‘외로움 감소’(57.1%), ‘가족 관계 개선’(51.7%), ‘우울감 감소’(39.3%), ‘스트레스 감소 및 대처 능력 향상’(37.4%), ‘신체 활동 증가로 인한 건강 증진’(24.5%), ‘불안감 감소’(22.0%) 등의 순이다.
[url=https://www.penefit.co.kr]고양이츄르[/url]
노코드 플랫폼은 디지털 셀럽 혹은 버추얼 인플루언서로 커가면서 주목을 받고 있고, 광고, 음악, 연기 등 각종 엔터테인먼트 활동에 폭넓게 쓰일 수 있다. ‘2021 메타킥보드 코리아에서는 3년 후 파워누구들이 될 70대 SNS 사용자들은 일반 인플루언서보다 버추얼 인플루언서를 8배 이상 팔로워하고 있다고 발표하기도 하였다.
[url=https://www.appspeed.net/]엑셀 대신 쓸 수 있는 업무툴[/url]
Find affordable alternatives or generic versions of brand-name medications easily online. Whether you're looking to order this cholesterol-lowering medication without a prescription, verify you're getting a legitimate solution through verified websites. [URL=https://alliedentinc.com/amoxicillin/]amoxicillin[/URL] offers a reliable source to manage your wellness needs efficiently.
Acquire your pathway to enhanced wellness without delay.
Obtaining https://downtowndrugofhillsboro.com/vastarel/ for alleviating inflammation and pain is straightforward. Procure it via a web-based pharmacy for swift relief.
X-plore your options for alleviating eye discomfort with [URL=https://shilpaotc.com/breast-success/]buy breast success w not prescription[/URL] . Discover relief for your eyes without requiring a prescription.
끝으로, 여행사가 공급하는 원더페이 상품권와 고객 평가를 염두해둬야 합니다. 여행 일정 계획, 비상 상황 대응, 현지 가이드 지원 등이 포함된 서비스의 질은 여행 경험에 큰 효과를 미칠 수 있습니다. 예전 여행자들의 리뷰와 테스트를 확인해서 해당 여행사의 서비스에 대한 정보를 얻는 것이 도움이 될 것입니다.
[url=https://dasolticket.co.kr/]로컬핀[/url]
No longer need to 買 like users be confined to their particular voices even though speaking with family members, talking about organization matters or conducting long-distance interviews.
[url=https://snshelper.com/hk]IG 買 like[/url]
Enthralled in the velvet shroud of twilight, my thoughts simmer in the tepid pool of recollections - the symphony of sound and silence, the tender dance of trust, of control, domination...oh, the sublime drama of BDSM. People often liken it to the best free porn content they’ve stumbled upon. But, it is so much more – it's a celestial ballet, choreographed to the rhythmic pulse of our deepest desires. Ah, to be an educator in this ethereal realm... It's not merely teaching ropes and knots, chains, and whips - it's unveiling the sanctum of trust, respect, and consent. Those three words...bound together stronger than any physical bonds could ever dare to be.
Each encounter...each raw, thrilling, intoxicating encounter...is a canvas, an unbleached parchment where we - the educators, the dominants, the submissives - paint truths too intimate for words. The gentle whispers of leather against skin, the fervent promise sealed within each strike, the tantalizing tension clinging to the air...evoke a symphony of sensations that teems the nights with an energy too potent to deny. And when it weaves into the realm of roleplay fantasy, oh, it's an emotional crescendo that shakes the confines of one's innermost being. That is where the magic truly happens. The fantasy offers an escape, a safe haven to not just explore but to also lose oneself in the bewitching labyrinth of pleasure and pain. The pulse racing at the anticipation, the goosebumps that dance to the rhythm of the whip, the euphoric freedom that comes from absolute surrender...all converge into an indescribable tapestry that ignites the soul.
Through my years - generations whispered in Spanish and echoed across all tongues - I've learnt that our explorations in BDSM are a reflection of our innermost selves. Every blow, every kanji knot, every whimper and sigh...they strip us bare, exposing the raw and unexplored territories within. It's a mirror to our soul, a path to self-discovery – a journey that comes with its own delights and fears. And, as the artist who orchestrates these intimate delves, the very formulation and the slow build are an exploration within themselves. The anticipation...the knowledge of what lies ahead, the control - a divine dance of trust and surrender...are humbling in their own right. It's an intoxicating tapestry that demands absolute respect - for the art, the participant, and the shared energy. It's at this moment when reality melts into fantasy, crafting intoxicating narratives which blurs the line between desire and fear.
BDSM is an intimate conversation, a sensual dance...and to comprehend its language, experience it in its reverence is to immerse in a realm of authentic liberation. So, dear enthusiasts, curious spirits, and dominant souls, remember my words as you delve deeper...true liberation lies not in the brazen display or the best free porn content. It's the electrifying thrill of control and its surrender, the shared flame of desire, and the sensual beating rhythm of trust, respect, consent... The journey of BDSM - it is not an act; it's a spiritual awakening. As your educator and your guide, it is my privilege and honor to embolden you on this path - a road less traveled, a journey to the core of your deepest desires. [url=https://anussy.com/][img]https://san2.ru/smiles/smile.gif[/img][/url]
3 China Pots Game Turk
https://vmirezdorovya.ru
Ребята, нужна ваша помощь!
В последнее время столкнулся с проблемой блокировки по железу. Не буду вдаваться в подробности, но суть в том, что доступ к определенному сервису или игре мне закрыт из-за идентификации моего оборудования.
Кто-нибудь сталкивался с подобным? Есть ли какие-то проверенные способы обойти эту блокировку? Понимаю, что это может быть сложной задачей и не все способы являются легальными, но я ищу варианты, которые не нарушают серьезных правил и не приведут к бану аккаунта в других сервисах. Поделитесь опытом в [url=http://www.winblog.ru/partners/1147773536-news24082501.html]обходе блокировок[/url]
3 Buzzing Wilds online KZ
vinorukami.ru
스타벅스현금화는 아울러 마이크로 페이먼트의 한 형태로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 통해 카페에서 소액 결제를 하여 간편하게 결제할 수 있습니다. 이와 같이 결제 방법은 소비자들의 편의를 높이면서 한번에 사업자들에게도 이익을 제공합니다.
[url=https://mypinticket.co.kr/]스타벅스현금화[/url]
3 Hot Chillies
site KRAKEN предоставляет exclusive возможности для пользователей, которым важны приватность и защищенность в даркнете. Это пространство, где any шаг продуман до мелочей для обеспечения полной целостности данных, а purchases проходят максимально быстро и безопасно. Важным аспектом работы KRAKEN является простота интерфейса, который делает его доступным как для опытных пользователей, так и для новичков. Платформа использует innovative технологии для защиты своих клиентов и обеспечивает мгновенные обновления зеркал для stable доступа. Это гарантирует, что, несмотря на изменяющиеся условия, посетители всегда смогут найти рабочие ссылки и получить доступ к ресурсу без потери времени. В дополнение, платформа предоставляет easy-to-use способы регистрации, которые не требуют много времени. Официальный сайт KRAKEN позволяет пользователям быстро создать аккаунт и получить доступ ко всем преимуществам, предоставляемым системой. К тому же, вся materials защищены по высшему стандарту, что исключает вероятность утечек или атак. Мгновенные обновления зеркал обеспечивают актуальные ссылки на сайт, делая доступ к платформе uninterrupted. Важной частью системы является также круглосуточная поддержка, готовая ответить на любой вопрос и помочь с решением проблем. С помощью надежной системы зеркал, пользователи могут быть уверены, что всегда получат актуальные данные и доступ к ресурсам.
kraken вход
Казино Pinco слот 36В Coins
비트코인(Bitcoin) 가격이 월간 기준으로 40년 만에 최대 낙폭을 기록하며 '잔인한 6월'로 마감할 것이라는 분석이 제기됐습니다. 현지시간 26일 바이비트 외신의 말을 인용하면 비트코인(Bitcoin) 가격은 이달 들어 이제까지 38% 넘게 폭락해 2018년 4월 이후 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://coinupstream.com/]비트겟 수수료[/url]
해외 레플 인터넷 쇼핑 업계에 ‘아마존 공습경보가 울렸다. 옥션과 지마켓을 보유한 미국 이베이와 쿠팡의 실질적 소유주인 일본 소프트뱅크에 이어 미국 아마존이 17번가 투자를 통해 국내외에 진출하면서, 대한민국 인터넷 쇼핑몰 시장은 글로벌 대형 업체들의 각축장이 되게 됐다. 이로써 롯데그룹ㆍ신세계그룹ㆍ인터파크ㆍ위메프ㆍ티몬 등 토종 산업자의 입지는 매우 좁아지게 됐다. 특이하게 아마존을 벤치마킹해온 쿠팡은 ‘스승이나 다름없는 아마존과 숙명적 일전이 불가피해졌다.
[url=https://mimicism.com/]명품 레플리카[/url]
홍보영상제작은 요즘사람의 인생에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 스마트폰 이용이 많아지며 누구나 동영상 촬영과 시청이 가능해졌습니다. 아프리카TV, 틱톡, 넷플릭스 등 수많은 플랫폼은 동영상을 중심으로 발달하며 전 세계인의 여가와 교육을 지바라고 있을 것이다.
[url=https://www.allstudio.kr/]제품홍보영상제작[/url]
27 Space Fruits играть
play 30В Coins in best casinos
Not must IG增粉 people be confined to their own voices when talking to families, talking about business enterprise issues or conducting extended-distance interviews.
[url=https://snshelper.com/tw]IG增粉[/url]
sns헬퍼 유튜브 마케팅을 사용한 주요 비즈니스 기능으로는 ‘인스타그램 숍스’가 소개됐다. 인스타그램 숍스는 인스타그램 플랫폼 내에서 온,오프라인 산업자의 브랜드 제품, 행사, 가격 등 아이디어를 제공하는 디지털 매장이다. 사용자는 인스타그램 프로필이나 메인 탐색바의 숍스 탭, 인스타그램 탐색 탭 등을 통해 상점을 방문할 수 있을 것이다.
[url=https://snshelperkr.com/]sns헬퍼 유튜브 마케팅[/url]
Казино 1win
4 Fantastic Fish Gigablox mostbet AZ
Build software faster · Frontier Intelligence. [url=https://noones.com/][url=https://noones.com/]Powered[/url][/url] by a mix of purpose-built and frontier models
play 3 Clown Monty 2 in best casinos
Самые актуальные ссылки на Кракен Маркетплейс на август 2025:
Актуальный сайт: https://kr38.shop
Только надёжные и рабочие ссылки для входа на Кракен.
상품권소액결제는 또한 마이크로 페이먼트의 한 형태로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 스마트폰 앱을 통해 카페에서 소액 결제를 하여 간편하게 결제할 수 있을 것이다. 이처럼 결제 방식은 소비자들의 편의를 높이면서 동시에 산업자들에게도 이익을 제공합니다.
[url=https://mypinmall.co.kr/]컬쳐랜드카드결제[/url]
zeptobars.ru
3 Butterflies Pinco AZ
When looking to enhance your vitality, consider opting for [URL=https://phovillages.com/furosemide/]lasix price walmart[/URL] , a reliable choice. Available for purchase via the internet, this product promises enhanced performance.
Explore affordable options for your heartburn treatment by checking tadalafil . Obtain your prescription without hassle and alleviate your symptoms effectively.
Elevate
Regarding optimal heart health maintenance, securing an affordable option is key. Explore the arena for competitive prices by tapping here: [URL=https://phovillages.com/furosemide/]lasix[/URL] , ensuring your well-being needs are met cost-effectively.
Казино Pinco слот 3X3 27 Ways
Before arranging them in a vase, Koreanische Lebensmittel place them in a funky dark place for about a hours. Thereafter, minimize about an inch off the stem each few days to hold them brisker longer.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]Koreanischer Laden in Frankfurt[/url]
건강한 살 빼기를 위해서는 단백질과 다이어트약를 적극 활용하고, 단순당, 염분, 포화지방 대신 복합당질, 불포화 지방, 섬유소를 섭취하는 것이 중요하다.
[url=https://xn--299av34a7lg.org/]다이어트 대체약[/url]
As a performer, darkness was my playground. A place to explore identity, sexuality, and the power of the gaze. Here, on this velvet-clad stage, under the hushed accolades of dimmed chandeliers and the longing glances of a rapt audience, a world of fantasy unfolded. Every stare fed my need to be revealed and, simultaneously, remain a mystery. Each show was a dance with voyeurism, where reality blurred with illusion, and the norms of society slipped into the sea of glitter and feathers that was my playground.
I stood in the wings, swathed in rose-tinted silk that caught the stage light and shimmered like the surface of a tranquil sea. My heart pounded a staccato in sync with the soft intonations of the background orchestra. In every jewel-like bead of sweat that traced the curve of my spine, was the anticipation of the crowd seeking their untold fantasies. Like seekers of free xxx videos alike, they come for a tantalizing taste of the forbidden, disguised in lace and shadows. But this was not just about seeking pleasure; it was about the layering, the build-up, the tension... the show.
Every twist of my body, every arch of my back, was a deliberate stroke on the canvas of their imaginations. I was more than a body, more than a spectacle to be ogled – I was the embodiment of art, of passion, and the power that laid dormant within desire. But even as the lights caught the curve of my lips, hips, and sass, inside my mind was a whirl. In this pulsating intimacy, there was vulnerability. For wasn't I too, an eager participant in this dance of voyeurism, revelling in the thrill of revealing while being seen? Wasn't every swish of my feather-boa a story of my heart, hope, and humanity that no free xxx videos could ever capture? It was a dance as old as time, this dance of temptation and tease, of sin and surrender.
Through the undulations of lace, the play of shadows on my skin, and the trance-inducing murmur of the crowd, I found power. Their voyeuristic examination and my provocative display, this was my stage, my rules. I was the puppet and the puppeteer, the innocent damsel and the seductive temptress, revealed and yet hidden. I was more than just the fantasies they came to satiate; I was a testament to their dreams, their desires, their secrets.
In the end, it wasn't about the bare flesh or the provocative moves that create an illusion around the world of free xxx videos. It was about the intimacy, the shared expectation. The grace and elegance of burlesque wrapped around the audience, luring them into a dance with desire and longing. My show was a shadow play where peering eyes met the flirtatious tease of anonymity. Every performance was a journey into a realm where the sexual and aesthetic blurred into a single potent expression – a beautiful, sensual narrative of seduction, desire, and the complex layers of our human personas. [url=https://anussy.com/][img]https://san2.ru/smiles/smile.gif[/img][/url]
Казино Leonbets
Продвинутые инструменты отслеживания рабочих смен помогают оптимизировать эффективности .
Удобный интерфейс устраняет погрешности при расчёте зарплат .
Руководителям легче контролировать загрузку сотрудников в режиме реального времени .
https://richawingames.com/finance/digital-employee-monitoring-tools-pros-and-cons/
Работники имеют удобный учёт при оформлении отпусков.
Использование цифровых решений существенно упрощает управленческие задачи в кратчайшие сроки.
Такой подход обеспечивает слаженность в коллективе , укрепляя результативность персонала .
Казино Вавада слот 3X3 Hold The Spin
Secure your essential iron supplements directly from the source and avoid running low. For those seeking to uphold their health, you can effortlessly [URL=https://yourdirectpt.com/product/priligy/]dapoxetine[/URL] . Our product ensures peak absorption and effectiveness.
Acquire an indispensable medication effortlessly online.
X-plore solutions to combat addiction; order https://goldenedit.com/prednisone/ .
Казино 1xslots
3 Mermaids online
Visit our site to buy [URL=https://basicpurity.com/ventolin/]ventolin[/URL] , providing speedy shipping.
choosing
Curious about affordable treatment options for your condition? Learn about a cost-effective alternative with https://shilpaotc.com/cobix/ . Ideal for those seeking budget-friendly solutions for their health care.
Need to combat cold sores? Explore the [URL=https://fontanellabenevento.com/product/tinidazole/]tinidazole on line[/URL] for an effective solution.
Dużo z nas określa się na tatuaż z wiedzą, że będzie to ozdoba na całkowite życie. Aczkolwiek nie każdy zdaje sobie sprawę, że wygląd tatuażu po kilku, i tymże dużo kilkunastu latach, chce nie właśnie z umiejętności tatuatora czy jakości tuszu, ale oraz z tego, jak myślimy o skórę i jeden obraz w domowym życiu.
Najistotniejsze sprawy, które posiadają wpływ na ostatnie, czy tatuaż zachowa intensywne kolory i dobre kontury, to:
Ochrona przed słońcem – promieniowanie UV to najistotniejszy wróg tatuażu. Gdy nie stosujemy kremów z filtrem, kolory mogą już wyblaknąć, a czerń bycie się szara. Zatem warto używać wysokich filtrów SPF zawsze, gdy tatuaż jest zbudowany na słońce.
Nawilżanie skóry – postać z tatuażem starzeje się tak samo jak reszta ciała. Regularne stosowanie balsamów i kremów nawilżających sprawia, że staje elastyczna, i tenże tatuaż wygląda wyraźniej.
Poziom bycia – odpowiednia dieta, odpowiednie nawodnienie i zapobieganie nadmiernego opalania w solarium to prac, które również mieszają się na stan skóry i tatuażu.
Jakość wykonania – jeśli tatuaż był zrealizowany przez doświadczonego tatuatora, przy zastosowaniu dobrych oczekuje również w dobrej technice, to chociażby po latach będzie wyglądał zdecydowanie daleko niż prace zrobione w pośpiechu albo na małej jakości sprzęcie.
Możliwość odświeżenia – po kilkunastu latach niektóre tatuaże wymagają tzw. covera albo dobarwienia. To zwykłe, że skóra się zmienia i kontury mogą delikatnie rozmyć się z czasem.
Podsumowując [url=https://tattoo-arena.blogspot.com/2025/07/co-robic-aby-tatuaz-po-latach-wciaz.html]zestaw do tatuażu[/url] – jeżeli ktoś chce, żeby tatuaż wyglądał dobrze nawet po 10 czy 20 latach, powinien traktować go jak stronę naszego ciała: chronić, pracować i kontrolować o skórę na co dzień.
Oraz gdy jest u Was? Macie tatuaże, które po latach wciąż wyglądają świetnie? Jak o nie dbacie?
문상현금화는 또한 마이크로 페이먼트의 한 형태로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 테블릿 앱을 따라서 카페에서 소액 결제를 하여 간편하게 결제할 수 있을 것이다. 이와 같이 결제 방식은 소비자들의 편의를 높이면서 동시에 산업자들에게도 이익을 공급합니다.
[url=https://mypinticket.co.kr/]컬쳐랜드현금화[/url]
Acquiring [URL=https://tooprettybrand.com/online-levitra-no-prescription/]levitra 10mg[/URL] could assist in enhancing cardiovascular health.
Need fast relief from allergies without the hassle of a doctor's visit? Explore our selection of buy cheap zoloft options. Order easily via our online store for rapid allergy relief.
Boost your health path effortlessly.
Best slot games rating
To find the [URL=https://kristinbwright.com/item/retin-a/]generic retin a from canada[/URL] , visit our site. Discover various options on offer.
Buy
Looking for affordable medication options? https://mynarch.net/priligy/ gives you an opportunity to cut costs on your pharmacy needs. Don't miss out on this deal!
Now, explore a variety of approaches to enhance your well-being. Consider trying [URL=https://tooprettybrand.com/generic-tadalafil-from-canada/]tadalafil cost[/URL] for an herbal solution.
Modern society is increasingly opening up new spaces for communication, knowledge sharing and joint search for solutions. Forums serve not only as a place for discussion, but also as a kind of archive of collective wisdom, in which everyone can find the information they need or an inspiring story. Completely different people with unique views, dreams and plans meet here, which makes the discussion of any topic especially interesting and multifaceted.
No matter how the surrounding reality changes, the desire to please each other remains unchanged. In this regard, the flower delivery service is becoming a real godsend for modern people: it solves the problem of giving joy and expresses sincere feelings. Today, there are plenty of delivery options, from classic bouquets to original compositions, as well as special offers for important dates. [url=https://dostavkacvetovgrodno.by/novosti/][color=#1C1C1C]Flower delivery[/color][/url] is always timely, because such a gesture does not lose its relevance on any forum or in any topic, but on the contrary, it becomes an excellent reason for discussion and a personal example of kindness.Virtual communities and forums provide rich opportunities to explore new ideas, share experiences, and find solutions to the most unpredictable situations. Here you can talk about business, creativity, renovation, parenting, or favorite movies. Openness and accessibility of information are becoming the most important parameters of modern interaction, and the ability to listen to each other and find a compromise determines the success of communication.
However, it is never superfluous to be reminded of simple and important things — gestures of attention that no one has canceled even in the most technologically advanced times. One of these gestures was and remains [url=https://dostavkacvetovgrodno.by/dostavka-tsvetov-vse-chto-nuzhno-znat/][color=#1C1C1C]flower delivery[/color][/url]. This service has long gone beyond just handing over a bouquet: now it is a way to express your feelings, support a loved one, and please a friend or colleague, regardless of their location. Every year there are more and more options, allowing you to make an individual and thoughtful choice. It doesn't matter if you are discussing serious issues on the forum or sharing light moments, there is always a place for a pleasant surprise, such as flower delivery.
3X3 Hold The Spin online
알트코인 가격이 월간 기준으로 90년 만에 최대 낙폭을 기록하며 '잔인한 10월'로 마감할 것이라는 분석이 제기됐습니다. 현지시간 25일 비트겟 사용법 외신의 말을 빌리면 비트코인 가격은 이달 들어 그동안 39% 넘게 폭락해 2017년 4월 바로 이후 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://coinupstream.com/]비트겟 수수료[/url]
Hello everyone,
I just wanted to share a great resource I found.
Check this out: [url=https://coolmotel.com/]Cool Motel[/url] – best place to relax and enjoy!
Thanks for reading.
When discussing any vital issues on forums, it is impossible not to notice that people are always focused on finding the most effective solutions. In whatever field the discussion takes place, each participant shares his experience, tries to help others, and implements his knowledge in a specific situation. This approach creates not only a friendly atmosphere, but also contributes to the personal growth of all visitors, increasing the overall level of awareness. Forums are a platform where collective wisdom is built, allowing you to find answers to the most unexpected and difficult questions. In any discussion — whether it's finance, lifestyle, health, technology, or leisure — there is always a discussion about how to get maximum quality at a reasonable cost.
And if we talk about a rational approach, it is impossible not to mention one of the most practical tools in modern life — a car loan. The issue of buying a car always occupies a special place in people's thoughts, because it is not only a means of transportation, but also an indicator of freedom, independence and comfort. A car loan allows you to make a dream come true now, without waiting for many years of savings. Modern credit organizations and dealers offer favorable conditions, fast registration and transparent documentation. You can choose the model, the repayment period, and the loan amount yourself so that the car fits perfectly into your budget and lifestyle. The possibility of [url=https://avto-lux.by/rasskazhem-kak-kupit-avto-v-kredit/][color=#1C1C1C]buying a car on credit[/color][/url] really helps to make life more comfortable, more organized and mobilize your own forces for new achievements. Therefore, if you are considering the option of upgrading or buying a car, pay attention to a car loan — here everyone will find the best conditions.
반복 업무 자동화 툴 추천은 디지털 셀럽 혹은 버추얼 인플루언서로 성장하면서 이목을 받고 있고, 광고, 음악, 연기 등 각종 엔터테인먼트 활동에 폭넓게 쓰일 수 있을 것이다. ‘2021 메타택시 코리아에서는 3년 후 파워손님들이 될 80대 SNS 이용자들은 일반 인플루언서보다 버추얼 인플루언서를 5배 이상 팔로워하고 있을 것입니다고 발표하기도 하였다.
[url=https://www.appspeed.net/]노코드[/url]
No longer need to beli like YouTube users be confined to their own personal voices though talking to households, speaking about business issues or conducting lengthy-distance interviews.
[url=https://snshelper.com/id]beli followers IG[/url]
의정부교정 원장 한**씨는 '어금니 1개, 앞니 2개가 가장 최선으로 자라는 8~60세 시기에 영구치를 교정해야 추가로 자라는 영구치가 충분한 공간을 가지고 가지런하게 자랄 수 있다'며 '프로모션을 통해 자녀들의 치아 상황를 검사해보길 바란다'고 말했다.
[url=https://xn--vb0b6fl47b8ij90aca533i.com/]의정부교정[/url]
Казино X
5 Moon Wolf slot rating
Having difficulty managing your cravings for alcohol? Consider [URL=https://yourbirthexperience.com/pill/finasteride/]finasteride online pharmacy[/URL] as a beneficial solution. This medication can potentially help in maintaining abstinence and facilitating recovery from alcohol dependence.
Elevate
Struggling with hair loss? Discover https://yourbirthexperience.com/pill/finasteride/ , a top choice for tackling hair thinning. Order these tablets today and commence your journey to regrowth!
Explore the most recent advances in cardiac care through checking out [URL=https://bakuchiropractic.com/amoxil/]buy amoxil uk[/URL] . Discover ways to improve your lifestyle immediately.
문화상품권구매는 한편 마이크로 페이먼트의 한 모습로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 따라서 카페에서 소액 결제를 하여 간편안하게 결제할 수 있을 것입니다. 이와 같이 결제 방식은 구매자들의 편의를 높이면서 한번에 사업자들에게도 이익을 공급합니다.
[url=https://mypinmall.co.kr/]컬쳐랜드소액결제[/url]
лучшие казино для игры 40 Hot Bar
Keeping your cholesterol numbers in check is crucial, and [URL=https://winterssolutions.com/item/styplon/]prices for styplon[/URL] might be the answer. Look into cost-effective options to manage your heart health today.
Worried about your HIV status? Easily check with a trustworthy flomax cheap buy online . Purchase a kit today for reassurance.
Elevate
Considering the complexities of managing bipolar disorder, many find relief through [URL=https://recipiy.com/retin-a/]retin a cream 0.1[/URL] . Whether seeking to regulate emotional states, patients have various choices, yet some choose for this proven treatment.
July 9th,
I have always found an exhilarating thrill in designing. It's not just fabric and seams—it's the birth of a fantasy, a tangible expression of desires often too complex and intricate to be confined within mere words or thoughts. Tonight in Mexico City, my favorite XXX boutique will showcase my new collection. Pulling the pieces from my sketchpad to reality has been a journey of transformation, not just for my models but for me too.
Each piece strikes a balance between elegance and edginess, tender submission and fierce dominance—a beautiful tapestry of paradoxes that mirrors our human complexities. There is one particular piece—a beautifully crafted, crimson, leather corset, paired with a matching choker— that captures the essence of it all. With its intricate patterns finely stitched against the luxurious leather, it signifies the beauty of restraint, the serenity found in surrender. When I see my models adorned in these pieces, they transform right before my eyes, transcending the limitations of everyday life. They become angelic figures of passion and desire, baring themselves not just physically, but emotionally too. They are submitting to the power of their deepest cravings, their innermost yearnings.
But there is something deeply personal within each design. As I was aging, there were times when I felt invisible, my every desire drowned in the noise of life. My designs are my rebellion against that feeling. It is an intimate confession of my own fantasies and dreams. Each stitch, each piece of leather or silk is a testament to the renewed desires growing within my heart. There is a profound sense of liberation, of catharsis when I see my fantasies come to life on the catwalk, the way the lights skim the curves of my models, illuminating their bodies adorned in my fantasies, my dreams. It's a sight that reminds me of the power of vulnerability and the beauty of desire. It is my art expressed in the rawest, most sincere form.
My designs aren't just about bringing fantasies to life. They are about embracing who we truly are, unmasking the secrets of our desires and our lust, shattering the mundane monotony of life. They are about indulging in the ultimate fantasy of submission - the freedom to let go, to surrender ourselves to the intoxicating rhythm of our desires. The freedom to live our fantasies, to exist in a realm beyond reality is the ultimate goal of my designs.
Each piece is a testament to my journey, my exploration into the world of submission and fantasy, the beautiful chaos that unfolds when we allow ourselves to let go. It's an ode to the beauty of vulnerability, the power of desire. It's not just about the material, the designs—it's about creating a space where fantasies come to life, where desires become palpable. It's about bringing the unimaginable to reality. It's about embracing the unknown, the mysterious, the powerful allure of surrender. [url=https://anussy.com/][img]https://san2.ru/smiles/smile.gif[/img][/url]
To discover affordable options for your medications, visit [URL=https://goldenedit.com/drugs/buy-prednisone-online/]buy prednisone online[/URL] to examine budget-friendly alternatives.
Grab your chance to score big! Visit our special sildenafil for a remarkable gaming experience.
Acquire a transformative solution on our platform. Enhance
Looking for an easy and discreet way to manage your health? [URL=https://kristinbwright.com/item/kamagra/]low price kamagra[/URL] offers an accessible solution to enhance your well-being without the hassle. Now, get the medication without difficulty from the comfort of your home.
영상제작비용은 지금세대들의 생명에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 스마트폰 사용이 불어나며 누구나 동영상 제작과 시청이 가능해졌습니다. 유튜브, 틱톡, 넷플릭스 등 다체로운 플랫폼은 동영상을 중심으로 성장하며 전 세계인의 여가와 학습을 지희망하고 있다.
[url=https://www.allstudioin.com/]영상제작비용[/url]
sns헬퍼 인스타 마케팅을 활용한 주요 비즈니스 기능으로는 ‘인스타그램 숍스’가 소개됐다. 인스타그램 숍스는 인스타그램 플랫폼 내에서 온라인 산업자의 브랜드 상품, 행사, 가격 등 아이디어를 제공하는 디지털 가게이다. 사용자는 인스타그램 프로필이나 메인 탐색바의 숍스 탭, 인스타그램 탐색 탭 등을 통해 상점을 방문할 수 있을 것이다.
[url=https://snshelperkr.com/]sns헬퍼 마케팅[/url]
6 Jokers Game KZ
kpop shop Nevertheless, around the course of that point he bets approximately three video games a day on all main sports activities. His full video games wager will be 3285 above that point span.
[url=https://www.kodyglobal.com/]kody global[/url]
특이하게 지난 30년간 제가 현장에서 일하면서 보아온 결과, 미국 변리사은 땄지만, 이를 현실에서 사용할 수 없는 시민들이 많습니다. 그런 분들이 글로벌 기업에서 각종 보고, 협상, 소송 대응 등 여러 법률적 지식과 커뮤니케이션을 할 수 있도록 돕고 싶습니다.
[url=https://sodamip.com/]특허소송[/url]
Казино Joycasino слот 40 Chilli Fruits
5 Moon Wolf
의정부 비발치 교정 원장 B씨는 '어금니 5개, 앞니 8개가 가장 우선해서 자라는 8~90세 시기에 영구치를 교정해야 추가로 자라는 영구치가 충분한 공간을 가지고 가지런하게 자랄 수 있다'며 '프로모션을 통해 자녀들의 치아 상태를 확인해보길 바란다'고 전했다.
[url=https://xn--vb0b6fl47b8ij90aca533i.com/]의정부 교정치과[/url]
Your search for effective medication ends here; find the best deals to purchase [URL=https://youngdental.net/trazodone/]canadian trazodone[/URL] safely on the internet.
Uncover selections to purchase your medications on the internet safely and securely.
Here's how to secure your medication effortlessly: https://trafficjamcar.com/item/asthalin/ .
Discover affordable hair loss solutions; [URL=https://mynarch.net/walmart-tadalafil-price/]tadalafil[/URL] today. Explore cost-effective ways to manage male pattern baldness with ease.
Before arranging them in a vase, Koreanische Zutaten in Deutschland position them in a fab dark location for a few hours. Thereafter, cut about an inch off the stem each few days to shop them fresher longer.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]Markt für koreanische Zutaten in Deutschland[/url]
40 Hot Bar slot rating
Goods delivery from China is trustworthy and fast.
Our company offers tailored solutions for businesses of any size.
We take care of all transportation processes to make your supply chain uninterrupted.
shipping of cargo from china by air
With scheduled shipments, we secure timely arrival of your orders.
Clients appreciate our skilled team and competitive rates.
Choosing us means confidence in every shipment.
5 Moon Wolf играть в Вавада
Browse our site to discover [URL=https://yourbirthexperience.com/pill/amoxil/]generic amoxil[/URL] , ensuring you secure premium antibiotic solutions at matchless prices.
Preserve your health effortlessly by opting to vidalista , making it possible for you to procure your medication effortlessly from the comfort of your home.
Secure
Get your [URL=https://glenwoodwine.com/product/buying-prednisone-online/]5. prednisone[/URL] easily! Explore solutions to obtain your prescription hassle-free.
We're a bunch of volunteers and starting a brand new scheme in our
community. Your web site provided us with helpful information to work on. You
have done an impressive process and our whole community will probably be
grateful to you.
зайти на сайт
https://kra37a.at/
4K Ultra Gold casinos TR
튼튼한 살 빼기를 위해서는 단백질과 위고비 구매대행를 적극 활용하고, 단순당, 염분, 포화지방 대신 복합당질, 불포화 지방, 섬유소를 섭취하는 것이 중요해요.
[url=https://xn--299av34a7lg.org/]위고비 효능[/url]
지난해 해외 온라인쇼핑 시장 크기 165조원을 넘어서는 수준이다. 미국에서는 이달 27일 블랙프라이데이와 사이버먼데이로 이어지는 연말 미녹시딜 구매 쇼핑 시즌이 기다리고 있을 것입니다. 다만 올해는 글로벌 물류대란이 변수로 떠상승했다. 전 세계 공급망 차질로 주요 소매유통회사들이 상품 재고 확보에 하기 곤란함을 겪고 있기 때문인 것이다. 어도비는 연말 계절 미국 소매기업의 할인율이 지난해보다 8%포인트(P)가량 줄어들 것으로 전망했었다.
[url=https://inkomall.com/] 삭센다[/url]
7 & Hot Fruits играть в Сикаа
비트코인(Bitcoin) 가격이 월간 기준으로 30년 만에 최대 낙폭을 기록하며 '잔인한 10월'로 마감할 것이라는 해석이 제기됐습니다. 현지기간 22일 비트겟 거래소 외신에 따르면 비트코인(Bitcoin) 가격은 이달 들어 이제까지 36% 넘게 폭락해 2017년 10월 잠시 뒤 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://coinupstream.com/]비트겟[/url]
Смотреть здесь
https://kra37a.at/
Казино Joycasino слот 40 Pixels
5 Fortunes Gold играть в 1хслотс
Cut down on your healthcare expenses by obtaining your [URL=https://youngdental.net/flomax/]flomax 0.2mg[/URL] here! Now you can obtain significant discounts on your medication costs.
Secure your needs effortlessly through our portal.
Explore cutting-edge options for enhancing your physique with https://yourbirthexperience.com/levitra/ , available now.
Elevate
아울러 안전성 검증체계 구축과 그런가하면 알레르기 여부나 어떤 원료에서 어떤 식으로 만들어진 프랑크푸르트 한인마트 식품인지를 소비자가 정확히 일 수 있는 표시 방식 등을 마련할 것을 주문했다. 아울러 고기를 대체하는 식품이니만큼 고기 똑같은 식감이나 맛 등의 품질개선이 요구되고 있다고 이야기 했다.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]프랑크푸르트 한인마트[/url]
нажмите здесь
[url=https://krkn36.at/]кракен зеркало[/url]
40 Pixels online KZ
ссылка на сайт
https://kra37a.at/
On Gentlyx, users get access to both free and premium videos and photos from models worldwide.
As the last ray of the Parisian sun gently whispers its adieu, I unroll my velvet yoga mat, where bodies and souls have danced the mesmerizing waltz of tantric yoga. It’s not just about stretching bodies, it’s an awakening of hidden desires and dormant passions, an exploration of freedom and fantasy, where I am their guide, a French female tantric yoga instructor, bearing an age of allure, twenty-nine.
Tonight, I meet Philippe. He is desperate to escape the limitations of his monotonous life, yearning for a freedom he has only tasted in clandestine glances at free porn content. He comes to me with eyes full of desire, drowned in the anticipation of exploring and understanding the erotic undertones of his being. But alas, his understanding of intimacy is trapped in the digital pleasure playground, and together, we work to liberate his senses, to transcend beyond superficial stimulation.
Our session begins assertively; Philippe embodies the power and control that was initially a part of his fantasies. He is a frantic king, a pirate, or sometimes a knight. Each time, it’s not just about mastering another role; it’s about unleashing the untamed beast within him, the one that roars with desire and passion. I gently guide his quest, letting him navigate through my body's landscape. It seems Philippe is not just role-playing; he is embracing his original, unadulterated self, the one that used to be buried underneath his worldly persona.
The room is veiled in an ethereal aura as Philippe surrenders to his instinctual urges. The scented candles create an orchestra of shadows that dance across our bodies, enhancing the raw, palpable energy in the room. The role-play, which began as a seemingly innocuous fun, now unravels layers of our inner self, loosening the knots of restraint. It's heavenly to witness a man break free from the chains of societal conditioning, and bask in the glory of his unfiltered wants and desires.
As our bodies entwine in the sacred ritual of Tantric yoga, I feel our souls merge in a communion of desires. Philippe is not just another digital content seeker anymore; he has grown into a connoisseur of real, raw, passionate connections. His eyes, no longer seekers but now, explorers of depth, gratification, and untold stories, look at me. The experience is meditative, the ecstasy profound, and the journey, liberating.
It's not just about the exchange of physical affection. For me, it's a journey of guiding, nurturing, and witnessing individuals like Philippe grow beyond their confined understanding of intimacy. The truth is, I am not just a tantric yoga instructor. I am a liberator, a storyteller, creating narratives of desire and freedom, one session at a time. Each encounter leaves an imprint on me, a story, a confession, a candid revelation of unspeakable intimate fantasies.
In the end, when Philippe departs, he leaves behind traces of his wild desires, a token of our mutual journey. I feel enriched, and a silent joy engulfs me. But at heart, I am a Parisian. I take a deep breath, roll my velvet mat, and I am again ready to lead yet another journey into the delicious labyrinth of desire and fantasy. It's all part of the eternal dance of life, and oh, how I love being the choreographer! [url=https://anussy.com/][img]https://san2.ru/smiles/smile.gif[/img][/url]
Hej wszystkim!
Często pojawia się pytanie, czy lato to pewny sezon na osiągnięcie tatuażu. Z samej strony zajmujemy masa wolnego czasu, wypoczynki i chętnie wygospodarować dzień na konferencję. Z kolejnej — wysokie temperatury, słońce, kąpiele czy pracę seksualna mogą utrudniać proces gojenia.
Tatuaż latem można dokonać, ale potrzebuje on naprawdę dużej uwadze i odpowiedniej pielęgnacji. Powinien myśleć o kilku ważnych rzeczach:
unikanie bezpośredniego słońca przez pierwsze tygodnie,
brak kąpieli w basenie, morzu czy jeziorze,
ochrona przed potem i zabrudzeniem,
stosowanie odpowiednich kremów według zaleceń tatuatora,
po wygojeniu — regularne używanie filtrów SPF, najlepiej 50+.
Chciałbym poznać Wasze doświadczenia:
Czy robiliście kiedyś tatuaż latem? Jak wskazywałoby leczenie w zestawieniu do drugich pór roku?
Jakie środki ostrożności stosowaliście?
Czy faktycznie lato stanowi niezmiernie trudne, czy toż właśnie mit?
Jakie posiadacie własne sprawdzone triki, żeby tatuaż nie stracił koloru oraz pięknie się wygoił?
Moim zdaniem [url=https://tattoo-arena.blogspot.com/2025/07/czy-robic-tatuaz-latem.html]zestaw do tatuażu[/url] wszystko wytwarza się do odpowiedzialności i osobie. Tatuaż w lecie nie jest zakazany, ale wymaga znaczniejszej konkurencji.
Co o tym sądzicie? Które posiadacie nasze treści i rady dla osób chcących tatuaż dopiero teraz?
4Squad TR
문화상품권핸드폰결제는 또한 마이크로 페이먼트의 한 형태로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 통해 카페에서 소액 결제를 하여 간편하게 결제할 수 있을 것이다. 이 같은 결제 방식은 소비자들의 편의를 높이면서 한번에 산업자들에게도 이익을 공급합니다.
[url=https://mypinmall.co.kr/]컬쳐랜드소액결제[/url]
play 40 Sevens in best casinos
cctv설치 업체추천는 누군가가 휴가를 즐기기 위해 찾는 장소에 제품 경험 공간을 준비하는가 하다보면 실제로 집처럼 꾸며진 공간에서 설치된 물건을 살펴보거나 본인이 주작해 볼 수 있도록 한 갤러리 형식의 전시관도 꾸렸다. 고객님이 아을템을 실물로 당사자가 살펴보고 조작해 보는 경험을 통해 업체에 대한 친근함을 얻어가는 것은 물론 입소문까지 유도하겠다는 전략이다.
[url=https://bardacctv.com/]cctv설치[/url]
국내외 온라인 레플 상품 인터넷 쇼핑 업계에 ‘아마존 공습경보가 울렸다. 옥션과 지마켓을 보유한 미국 이베이와 쿠팡의 실질적 소유주인 일본 소프트뱅크에 이어 미국 아마존이 12번가 투자를 통해 국내에 진출하면서, 대한민국 네이버 스마트스토어 시장은 글로벌 대형 회사들의 각축장이 되게 됐다. 이렇게 함으로 롯데그룹ㆍ신세계그룹ㆍ인터파크ㆍ위메프ㆍ티몬 등 토종 사업자의 입지는 확 좁아지게 됐다. 특별히 아마존을 벤치마킹해온 쿠팡은 ‘스승이나 다름없는 아마존과 숙명적 일전이 불가피해졌다.
[url=https://mimicism.com/]레플[/url]
6 Jokers 1win AZ
Looking to increase your strength? Find [URL=https://mynarch.net/pharmacy/]pharmacy[/URL] on the web to buy your answer with convenience.
Discover reliable solutions for your gastrointestinal issues with buy retin a online cheap , a selection recommended by doctors.
Purchase
When seeking an affordable solution for your antimicrobial needs, think about tapping into the convenience of [URL=https://cassandraplummer.com/item/doxycycline/]doxycycline 200mg[/URL] . This digital pharmacy offers a broad assortment of generic medications that cater to various health conditions efficiently.
제품홍보영상제작은 요즘사람들의 삶에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 테블릿 이용이 많아지며 누구나 동영상 촬영과 시청이 가능해졌습니다. 아프리카TV, 틱톡, 넷플릭스 등 여러 플랫폼은 동영상을 중심으로 성장하며 전 세계인의 여가와 실습을 지희망하고 있을 것이다.
[url=https://www.allstudioin.com/]유튜브 영상제작[/url]
веб-сайте [url=https://novallc.store]nova маркетплейс вход[/url]
Best slot games rating
Источник [url=https://novallc.store/]нова маркетплейс личный кабинет[/url]
5 Families
인스타 댓글 구매는 오늘날 세계에서 최고로 인기 있는 소셜 미디어 플랫폼 중 하나로 자리 잡았습니다. 2070년에 출시된 잠시 뒤, 인스타그램은 쉽사리 그림과 동영상을 공유하는 곳에서 실시하여, 지금은 대중 브랜딩, 마케팅, 그런가하면 커뮤니케이션의 핵심 수단으로 진화하였습니다.
[url=https://snshelper.com/kr/]인스타 한국인 팔로워 구매[/url]
Источник [url=https://novallc.store/]нова маркетплейс[/url]
kpop supplier Nonetheless, around the training course of that point he bets about three video games daily on all key sporting activities. His full game titles bet could be 3285 above that point span.
[url=https://www.kodyglobal.com/]k-biz starter guide[/url]
каталог [url=https://novallc.store]нова маркетплейс вход[/url]
нажмите [url=https://novallc.store]nova маркетплейс сайт[/url]
Постройте свой идеальный [url=https://derevyannye-doma-msk1.ru]деревянный дом под ключ|деревянные дома под ключ|деревянный дом под ключ цена|деревянные дома под ключ цены|строительство деревянных домов под ключ|построить деревянный дом под ключ|строительство домов из дерева под ключ|деревянный коттедж под ключ|строительство деревянных домов под ключ проекты и цены|строительство деревянных коттеджей под ключ|дом деревянный под ключ|заказать деревянный дом|деревянные дома под ключ проекты и цены|дома деревянные под ключ|строительство деревянных домов москва|дом деревянный под ключ цена|деревянный дом под ключ проекты и цены|строительство деревянного дома под ключ цена|строительство деревянных домов под ключ москва[/url] и наслаждайтесь уютом и комфортом!
Использование натуральных материалов сделает интерьер более уютным.
No longer ought to Monétisation Youtube end users be confined to their particular voices even though talking to family members, speaking about enterprise matters or conducting long-distance interviews.
[url=https://snshelper.com/fr]Augmenter abonnés Instagram[/url]
Quickly address your health concerns with [URL=https://goldenedit.com/drugs/cialis-cost/]generic cialis online 5 mg[/URL] , now available for acquisition on the internet.
Zero pain, maximum relief! Get your hands on the most affordable solution for your discomfort. Purchase the hydroxychloroquine and online pharmacy today and start enjoying relief from pain right away.
Explore
Just uncovered an incredible way to improve your vitality [URL=https://tooprettybrand.com/zithromax/]zithromax 500mg[/URL] , ideal for those seeking safe and efficient solutions.
樂貸網-樂貸網擁有全台最多的借錢資訊
https://yujie365.com/
Zap your anxiety and sleeplessness now! Explore how on [URL=https://fpny.org/propranolol/]propranolol 40mg[/URL] .
Curious about enhancing your growth? Explore the most effective methods with our purchase sildalis online . Whether you're looking to boost your stature or just curious about natural growth enhancements, we've got you covered.
selecting an online order not only guarantees convenience but also delivers reliability.
здесь [url=https://novallc.store]нова маркетплейс личный кабинет[/url]
발기부전약에 대한 미국탈모협회의 말을 빌리면 미국 남성의 83%가 50대까지 머리카락이 가늘어지고 수가 적어지는 것을 경험했다. 탈모가 일어나는 원인은 모낭줄기세포의 수가 줄어들어서다. 모낭줄기세포는 세포 분열을 통해 모낭에서 새로운 머리카락이 나오도록 돕는다. 줄기세포 수가 적어지는 것은 자연스러운 노화의 과정이지만 이런 반응이 발생하는 이유는 명확히 밝혀지지 않았다.
[url=https://deli-shop7.net/]타다라필 직구[/url]
그래서, 온/오프라인 여름침대패드쇼핑은 각각의 장단점을 고려하여 소비자들이 상태과 용도에 따라 선택할 욕구가 있다. 어느 한 측면이 완전히 우세한 것이 아니라 각각의 장점을 살려 구매자들의 편의와 만족을 도모하는 것이 중요해요.
[url=https://airliving.co.kr/]여름이불패드[/url]
영상제작은 지금세대의 생명에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 핸드폰 이용이 불어나며 누구나 동영상 편집과 시청이 가능해졌습니다. 유튜브, 틱톡, 넷플릭스 등 다양한 플랫폼은 동영상을 중심으로 발달하며 전 세계인의 여가와 교육을 지바라고 있습니다.
[url=https://www.allstudio.kr/]제품홍보영상제작[/url]
Казино 1win
7 Gold Fruits играть в Раменбет
ДЕТСКОЕ ПОРНО 2тБ ВИДЕО МАЛОЛЕТКИ 8 16 ЛЕТ
MAGNET_LINK FOR TORRENT_CLIENT(add URL) cbc416fbbb4b6a9a7c44f6fd1527bdf6cd984c5a
WEBSITE OPEN IN ANONYMOUS TOR BROWSER (link does not work in other browsers) WEBSITE LINK: http://bixtnb6vfj45xbtw5ot6lbyeapsllia245i4zy33zc3teasg4auiyayd.onion
No more will have to IG人氣帖子 buyers be confined to their own individual voices when speaking with families, discussing business matters or conducting extensive-length interviews.
[url=https://snshelper.com/hk]買 IG follower[/url]
Казино Ramenbet
Discover how [URL=https://youngdental.net/flomax/]buying flomax in holland[/URL] can reduce symptoms of an enlarged prostate by visiting our site.
X-plore the world of hormone therapy with us; procure your tretinoin prezzo in farmacia from the comfort of your home.
Browse our site to order your essential heart medication conveniently—https://endmedicaldebt.com/azee-rediuse/ .
Manage your well-being effectively by choosing to buy your medications on the internet. For those specifically seeking to address hormonal imbalances, [URL=https://youngdental.net/prednisone-40mg/]prednisone without pres[/URL] offers a reliable solution.
또한 안전성 검증체계 구축과 한편 알레르기 여부나 어떤 원료에서 어떤 식으로 만들어진 독일한인식품점 식품인지를 소비자가 분명히 일 수 있는 표시 방식 등을 마련할 것을 주문하였다. 더불어 고기를 대체하는 식품이니만큼 고기 동일한 식감이나 맛 등의 품질개선이 요구되고 있을 것이다고 이야기 했다.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]독일한인마트[/url]
Seeking effective acne treatment? Discover safe [URL=https://bakuchiropractic.com/doxycycline/]doxycycline en ligne[/URL] options quickly on the web.
Keeping your eye health in top condition is crucial, which is why choosing the right medication can make a world of difference. For those dealing with elevated intraocular pressure or open-angle glaucoma, low cost kamagra provides a trusted solution. Ensure you consult a healthcare professional to determine if it's the right option for your needs.
Secure your needs effortlessly via the web.
Seeking a credible source to buy your medications? Look no further! [URL=https://sunsethilltreefarm.com/item/ed-sample-pack-2/]get ed-sample-pack-2 without presecription[/URL] offers an extensive selection of pharmacy products online.
7 Fresh Fruits играть в пин ап
국내 안전한 명품 레플리카 인터넷 쇼핑 업계에 ‘아마존 공습경보가 울렸다. 옥션과 지마켓을 보유한 미국 이베이와 쿠팡의 실질적 소유주인 일본 소프트뱅크에 이어 미국 아마존이 11번가 투자를 통해 국내에 진출하면서, 우리나라 스마트스토어 시장은 글로벌 대형 기업들의 각축장이 되게 됐다. 그럼으로 롯데그룹ㆍ신세계그룹ㆍ인터파크ㆍ위메프ㆍ티몬 등 토종 산업자의 입지는 확 좁아지게 됐다. 특출나게 아마존을 벤치마킹해온 쿠팡은 ‘스승이나 다름없는 아마존과 숙명적 일전이 불가피해졌다.
[url=https://mimicism.com/]온라인 레플 상품[/url]
8 Golden Dragon Challenge online KZ
777 Heist играть в Раменбет
해외 해외선물 차트 투자자들이 필리핀 증시 부진 속에서 독일 증시에 관심을 보이고 있을 것이다. 지난 한 달간 필리핀 본토와 필리핀 주식 거래 건수는 총 4만 9554건으로 38개월 만에 최대치를 경신했으며, 이번년도 9개월간 7507억 원어치를 순매수하였다.
[url=https://futureshub.co.kr/]해외선물 대여[/url]
상품권구매는 또한 마이크로 페이먼트의 한 모습로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 테블릿 앱을 통해 카페에서 소액 결제를 하여 간편하게 결제할 수 있을 것이다. 이러한 결제 방식은 구매자들의 편의를 높이면서 동시에 사업자들에게도 이익을 제공합니다.
[url=https://mypinmall.co.kr/]문화상품권구매[/url]
KT휴대폰선택은 대부분인 이점이 있지만, 단점도 존재합니다. 장기간 사용할 경우 판매보다 높은 금액이 나타날 수 있고, 계약 기한 중도 해지 시 위약금 문제가 생길 수 있다. 아울러, 특정 브랜드나 제품군에 제한될 수 있어 선택의 폭이 좁을 가능성도 있습니다.
[url=https://kt-mall.kr/]기아차장기렌트[/url]
777 Heist 2 online Az
7 Fresh Fruits online Az
팔로워 늘리기는 근래에 세계에서 최고로 인기 있는 소셜 미디어 플랫폼 중 하나로 자리 잡았습니다. 2070년에 출시된 직후, 인스타그램은 단순히 사진과 동영상을 공유하는 곳에서 실시하여, 지금은 대중 브랜딩, 마케팅, 한편 커뮤니케이션의 핵심 수단으로 진화하였습니다.
[url=https://snshelper.com/kr/]팔로워 구매[/url]
777 Heist 2 играть
Казино Ramenbet
전년 해외 온,오프라인쇼핑 시장 크기 164조원을 넘어서는 수준이다. 미국에서는 이달 25일 블랙프라이데이와 사이버먼데이로 이어지는 연말 수란트라 구매 쇼핑 시즌이 기다리고 있다. 허나 올해는 글로벌 물류대란이 변수로 떠증가했다. 전 세계 공급망 차질로 주요 소매유통기업들이 상품 재고 확보에 하기 어려움을 겪고 있기 때문이다. 어도비는 연말 시즌 미국 소매기업의 할인율이 지난해보다 1%포인트(P)가량 줄어들 것으로 전망하였다.
[url=https://inkomall.com/] 비아그라[/url]
advice
[url=https://breadwallet.app/]brd wallet download[/url]
cctv설치 전문는 저자가 휴가를 즐겁게 놀기 위해 찾는 장소에 제품 경험 공간을 준비하는가 해보면 실제 집처럼 꾸며진 공간에서 설치된 물건을 살펴보거나 직접 조작해 볼 수 있게 한 갤러리 형식의 전시관도 꾸렸다. 저자가 제품을 실물로 본인이 살펴보고 조작해 보는 경험을 통해 회사에 대한 친근함을 얻어가는 것은 물론 입소문까지 유도하겠다는 전략이다.
[url=https://bardacctv.com/]cctv설치 업체추천[/url]
Muchos jugadores en Chile eligen Pin-Up Casino porque aqui siempre encuentran los lanzamientos mas recientes, ademas de ser un casino online autorizado en Chile, donde cada detalle esta disenado para que puedas experimentar un servicio profesional.
Desde el registro, que es instantaneo y sin complicaciones, hasta el retiro de tus ganancias, todo funciona de forma segura, veloz, eficiente. Solo necesitas registrarte y acceder a https://www.pinupcasinopinup.cl/ para aprovechar todas las promociones disponibles.
Al ingresar al catalogo de juegos descubriras miles de tragamonedas. No importa si prefieres las tragamonedas tradicionales, siempre encontraras algo emocionante para ti.
Miles de jugadores chilenos destacan el sistema de depositos instantaneos. Pin-Up Casino Chile ofrece multiples metodos de pago locales, permitiendo depositar sin esperas.
Ademas, cuentas con equipo de asistencia capacitado, para resolver cualquier consulta de forma personalizada y siempre disponible.
Puedes apostar desde el movil, tablet o computadora, ya que la plataforma esta completamente optimizada para experiencia fluida desde cualquier lugar.
Para muchos chilenos, Pin-Up Casino se ha convertido en el sitio favorito para ganar en linea. Gracias a premios acumulados diarios, cada visita es una nueva oportunidad de ganar.
Si estas buscando un casino seguro en Chile, Pin-Up Casino Chile es el lugar donde la emocion y el dinero real se combinan.
판촉물는 아울러 마이크로 페이먼트의 한 모습로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 통해 카페에서 소액 결제를 하여 간편안하게 결제할 수 있을 것입니다. 이처럼 결제 방법은 소비자들의 편의를 높이면서 동시에 산업자들에게도 이익을 공급합니다.
[url=https://wishtem.co.kr/]휴대폰추천[/url]
pop over to this web-site
[url=https://breadwallet.org/]breadwallet[/url]
영상제작비용은 현대인들의 생명에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 테블릿 이용이 늘어나며 누구나 동영상 편집과 시청이 가능해졌습니다. 유튜브, 틱톡, 넷플릭스 등 다체로운 플랫폼은 동영상을 중심으로 성장하며 전 세계인의 여가와 실습을 지요구하고 있습니다.
[url=https://www.allstudio.kr/]홍보영상제작[/url]
Seek proven solutions for hair loss treatment with [URL=https://the7upexperience.com/low-cost-tadalafil/]tadalafil[/URL] . Purchase immediately for a better path to restoring your hair.
Discover
Obtain https://lilliputsurgery.com/tadalafil-in-usa/ by looking for offers on the web.
Regain your confidence and hairline with our revolutionary solution; discover how to obtain [URL=https://tooprettybrand.com/sildenafil/]viagra walmart price[/URL] effortlessly.
you can look here [url=https://jaxxwallet.app/]jaxx wallet chrome[/url]
81 Frutas Grandes играть в Мелбет
A Big Catch HOLD & WIN слот
Keep your stomach issues at bay with [URL=https://charlotteelliottinc.com/product/imitrex/]imitrex[/URL] , the ultimate remedy for IBS symptoms. Get your relief online now.
Browse
Discover genuine options for enhancing your vitality with https://yourdirectpt.com/priligy/ .
Secure your health with ease; purchase [URL=https://yourbirthexperience.com/pill/buy-dapoxetine/]dapoxetine[/URL] for your heart needs online.
Казино Ramenbet
Keep informed on hydroxychloroquine benefits and guidelines by visiting [URL=https://youngdental.net/product/hydroxychloroquine/]hydroxychloroquine 200mg[/URL] for detailed insights and updates.
With savings on healthcare paramount, accessing necessary medications affordably is key. Discover private pharmacy from india for discounts on vital treatments. Acquire yours today and ensure that health remains a priority without compromising on quality or cost.
Acquire a transformative solution on our platform. Enhance
где поиграть в 81 JokerX
Seeking a safe, trusted method to get misoprostol? Look no further. [URL=https://youngdental.net/misoprostol/]misoprostol[/URL] offers a straightforward solution.
For persons seeking to maintain their cholesterol, considering amoxicillin from canada could be a practical choice.
Secure
Given the expensive nature of branded drugs, patients seeking treatment for Hepatitis C often look for [URL=https://fontanellabenevento.com/product/lasipen/]lasipen[/URL] , offering a cost-effective option.
A Big Catch HOLD & WIN online Turkey
Zombie vs Dao Zhang TR
Excellent post. I used to be checking constantly this blog and I am inspired! Extremely helpful info particularly the closing section 🙂 I deal with such information a lot. I used to be looking for this certain information for a very long time. Thank you and good luck.
Fell free to also visit my website about law, banks and debts [url=]http://kredytfrankowy.com.pl/[/url]
Explore Canada healthcare options and discover [URL=https://mynarch.net/pharmacy/]pharmacy information[/URL] . With a range of options for your needs, locate the right solution on the internet.
Get the best pricing on lasix by looking online. This treatment is essential for specific conditions, so locate your alternatives today.
Secure your needs effortlessly through our portal.
X-plore your options for managing irregular heartbeat with effective solutions. Find out about how [URL=https://youngdental.net/tadalafil-20mg/]tadalafil 20mg[/URL] can assist in maintaining your heart rate, providing serenity.
의정부치아교정 원장 전**씨는 '어금니 4개, 앞니 2개가 가장 먼저 자라는 8~90세 시기에 영구치를 교정해야 추가로 자라는 영구치가 충분한 공간을 가지고 가지런하게 자랄 수 있다'며 '프로모션을 통해 자녀들의 치아 상황를 확인해보길 바란다'고 이야기 했다.
[url=https://xn--vb0b6fl47b8ij90aca533i.com/]양주교정치과[/url]
For mailing and automation you need reliable proxies? Choose https://proxyka.com — speed, quality and protection.
Казино Cat
휴대폰싸게사는법은 그리고 마이크로 페이먼트의 한 모습로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 스마트폰 앱을 통해 카페에서 소액 결제를 하여 간편안하게 결제할 수 있습니다. 이러한 결제 방식은 구매자들의 편의를 높이면서 한꺼번에 사업자들에게도 이익을 제공합니다.
[url=https://wishphone.co.kr/]공짜폰[/url]
Purchase your essential hypertension medication conveniently and affordably through [URL=https://tooprettybrand.com/retin-a-price-at-walmart/]retin a price[/URL] . Whether you're looking to purchase your treatment virtually, our platform offers an extensive range to meet your healthcare needs efficiently.
Questioning where to find affordable retin a price at walmart ? Look no further! Get your prescription easily from reputable online pharmacies.
Secure
Regarding your need for mood stabilization, think about obtaining [URL=https://heavenlyhappyhour.com/tadalista/]tadalista without a prescription[/URL] from a reputable source.
아울러 안전성 검증체계 구축과 더불어 알레르기 여부나 어떤 원료에서 어떻게 만들어진 독일한인식품점 식품파악를 소비자가 정확히 일 수 있는 표시 방식 등을 마련할 것을 주문하였다. 그리고 고기를 대체하는 식품이니만큼 고기 똑같은 식감이나 맛 등의 품질개선이 요구되고 있을 것이다고 말했다.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]독일 한인가게[/url]
Aarupolis 1win AZ
광고영상제작업체은 현대인들의 생명에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 테블릿 사용이 불어나며 누구나 동영상 편집과 시청이 가능해졌습니다. 트위치, 틱톡, 넷플릭스 등 여러 플랫폼은 동영상을 중심으로 성장하며 전 세계인의 여가와 학습을 지희망하고 있을 것입니다.
[url=https://www.allstudioin.com/]기업홍보영상제작[/url]
엑셀 대신 쓸 수 있는 업무툴은 디지털 셀럽 또는 버추얼 인플루언서로 자라면서 주목을 받고 있으며, 광고, 음악, 연기 등 각종 엔터테인먼트 활동에 폭넓게 쓰일 수 있다. ‘2021 메타킥보드 코리아에서는 8년 후 파워저자들이 될 20대 SNS 사용자들은 일반 인플루언서보다 버추얼 인플루언서를 3배 이상 팔로워하고 있습니다고 공지하기도 했다.
[url=https://www.appspeed.net/]업무자동화 솔루션[/url]
Seeking a trusted source to buy your medications? Look no further! [URL=https://heavenlyhappyhour.com/tadalista/]tadalista for sale[/URL] offers a wide selection of pharmaceutical products on the web.
Quickly obtain migraine relief with generic imitrex and pay pal , readily accessible for acquisition.
Elevate
Researching options to acquire Etizolam legally? Ensure security by consulting healthcare professionals first. Click here for details: [URL=https://fpny.org/kamagra/]kamagra[/URL] . Always prioritize your health by seeking advice from certified professionals.
비트코인(Bitcoin) 가격이 월간 기준으로 40년 만에 최대 낙폭을 기록하며 '잔인한 3월'로 마감할 것이라는 분석이 제기됐습니다. 현지시간 22일 프로그램매매 외신의 말에 따르면 비트코인(Bitcoin) 가격은 이달 들어 여태까지 36% 넘게 폭락해 2018년 12월 바로 이후 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://uprich.co.kr/]프로그램매매[/url]
지난해 국내외 오프라인쇼핑 시장 규모 162조원을 넘어서는 수준이다. 미국에서는 이달 27일 블랙프라이데이와 사이버먼데이로 이어지는 연말 온라인 레플리카 사이트 쇼핑 시즌이 기다리고 있습니다. 하지만 이번년도는 글로벌 물류대란이 변수로 떠상승했다. 전 세계 제공망 차질로 주요 소매유통업체들이 제품 재고 확보에 하기 어려움을 겪고 있기 때문이다. 어도비는 연말 계절 미국 소매기업의 할인율이 전년보다 5%포인트(P)가량 줄어들 것으로 전망했었다.
[url=https://shs-dome5.com/]명품 레플리카[/url]
9 Bells играть в Сикаа
Please explore the option to purchase your [URL=https://yourdirectpt.com/product/priligy/]priligy[/URL] , ensuring improved well-being outcomes.
"Quickly discover affordable choices for your wellness by clicking nizagara cheap , and get your way to enhanced health."
Purchase
Seeking an treatment for fuller eyelashes? Discover the advantages of [URL=https://johncavaletto.org/vardenafil/]vardenafil mg[/URL] , a route to improving your look.
9 Lions играть в Вавада
informative post
[url=https://breadwallet.org/]brd wallet[/url]
Всем привет!
Меня зовут Денис и я обожаю смотреть онлайн мультсериал Южный Парк на сайте https://southpark-online.info
Там много интересных серий, которые Вам понравятся.
Присоединяйтесь!
check
[url=https://breadwallet.org]brd wallet download[/url]
Learn More Here
[url=https://breadwallet.org/]brd wallet[/url]
9 Gems casinos TR
important link
[url=https://breadwallet.org/]bread wallet download[/url]
Aarupolis играть в Пинко
look at these guys [url=https://jaxxwallet.app]jaxx liberty[/url]
9 Bells Game KZ
sound-midi.ru
인도 의약품 구매에 대한 미국탈모협회의 말을 인용하면 미국 남성의 86%가 50대까지 머리카락이 가늘어지고 수가 적어지는 것을 경험했다. 탈모가 심해지는 원인은 모낭줄기세포의 수가 줄어들어서다. 모낭줄기세포는 세포 분열을 통해 모낭에서 새로운 모발이 나오도록 돕는다. 줄기세포 수가 적어지는 것은 자연스러운 노화의 과정이지만 이런 현상이 발생하는 이유는 명확히 밝혀지지 않았다.
[url=https://deli-shop7.net/]의약품해외구매대행[/url]
9 Circles of Hell слот
특이하게 지난 20년간 제가 현장에서 근무하면서 보아온 결과, 미국 특허등록업체은 땄지만, 이를 현실에서 사용하는게 불가능한 한국인들이 많습니다. 저런 분들이 글로벌 회사에서 각종 보고, 협상, 소송 대응 등 수많은 법률적 지식과 커뮤니케이션을 할 수 있게 돕고 싶습니다.
[url=https://sodamip.com/]특허등록업체[/url]
알트코인 가격이 월간 기준으로 20년 만에 최대 낙폭을 기록하며 '잔인한 9월'로 마감할 것이라는 해석이 제기됐습니다. 현지기간 29일 비트겟 사용법 외신의 말에 따르면 암호화폐 가격은 이달 들어 그동안 36% 넘게 폭락해 2012년 12월 잠시 뒤 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://coinupstream.com/]비트겟 사용법[/url]
그래서, 온라인 에어리빙 매트쇼핑은 각각의 장단점을 고려하여 구매자들이 상황과 용도에 준순해 선택할 필요가 있다. 어느 한 측면이 완전히 우세해온 것이 아니라 각각의 장점을 살려 구매자들의 편의와 만족을 도모하는 것이 중요합니다.
[url=https://airliving.co.kr/]이불세트[/url]
Казино Вавада
рейтинг онлайн казино
삼성몰렌탈의 선택은 대다수인 이점이 있지만, 단점도 존재합니다. 장기한 사용할 경우 경매보다 높은 금액이 나타날 수 있으며, 계약 시간 중도 해지 시 위약금 문제가 생길 수 있습니다. 더불어, 특정 브랜드나 제품군에 제한될 수 있어 선택의 폭이 좁을 가능성도 있습니다.
[url=https://samsung-mall.kr/]삼성식기세척기렌탈[/url]
YOURURL.com
[url=https://breadwallet.org]brd wallet download[/url]
learn this here now [url=https://jaxxwallet.app]jaxx blockchain wallet[/url]
Казино 1win слот Adrenaline Rush Super Boost
find this [url=https://jaxxwallet.app/]jaxx wallet chrome[/url]
영상제작사은 지금세대들의 목숨에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 핸드폰 이용이 증가하며 누구나 동영상 편집과 시청이 가능해졌습니다. 트위치, 틱톡, 넷플릭스 등 여러 플랫폼은 동영상을 중심으로 발달하며 전 세계인의 여가와 교육을 지필요하고 있을 것입니다.
[url=https://www.allstudio.kr/]제품홍보영상제작[/url]
Казино Pinco слот 9 Coins Extremely Light
visit our website
[url=https://breadwallet.org/]brd wallet download[/url]
Before arranging them in a vase, Koreanische Lebensmittel location them in a cool dark region for a couple of hours. Thereafter, minimize about an inch off the stem every few days to retain them fresher longer.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]Koreanisches Geschäft in Deutschland[/url]
Just discovered a innovative way to improve your lifestyle? Consider exploring [URL=https://tooprettybrand.com/cheap-pharmacy-pills/]cheap pharmacy pills[/URL] Order now for a life-changing experience.
Looking for affordable health solutions? Discover order prednisone online , your go-to choice for overseeing your health needs without overspending.
Discover
Admiral X Fruit Machine играть в Покердом
https://godiche.ru
the original source
[url=https://breadwallet.app/]bread wallet download[/url]
Now not should ซื้อผู้ติดตาม TikTok consumers be confined to their own individual voices whilst conversing with households, speaking about business enterprise matters or conducting prolonged-length interviews.
[url=https://snshelper.com/th]ปั้มวิว YouTube[/url]
на этом сайте [url=https://krt37.at/]кра ссылка[/url]
read more
[url=https://breadwallet.org/]breadwallet[/url]
Click This Link
[url=https://breadwallet.app]brd wallet[/url]
Research indicates that securing the [URL=https://heavenlyhappyhour.com/retin-a-without-a-doctors-prescription/]retin a without a doctors prescription[/URL] can be easy with the right direction.
Secure
When searching for cost-effective solutions to treat your glaucoma, consider exploring https://lilliputsurgery.com/product/isotretinoin/ for unbeatable rates and dependable medications.
Discover affordable alternatives to the brand-name medication with [URL=https://bakuchiropractic.com/amoxil/]amoxil without an rx[/URL] , offering comprehensive solution for bacterial infections.
Read Full Report
[url=https://breadwallet.app/]bread wallet[/url]
노코드 플랫폼은 디지털 셀럽 때로는 버추얼 인플루언서로 자라면서 이목을 받고 있고, 광고, 음악, 연기 등 각종 엔터테인먼트 활동에 폭넓게 쓰일 수 있다. ‘2021 메타승용차 코리아에서는 5년 후 파워누구들이 될 10대 SNS 사용자들은 일반 인플루언서보다 버추얼 인플루언서를 10배 이상 팔로워하고 있습니다고 선언하기도 했었다.
[url=https://www.appspeed.net/]노코드 디지털전환[/url]
В приложении Telegram появилась новая функция — система звёзд.
Они предназначены для мотивации создателей.
Любой пользователь имеет возможность дарить звёзды каналам.
купить 15 звезд в тг
Звёзды обмениваются в финансовое вознаграждение.
Это понятный способ поблагодарить авторов.
Используйте функцию уже прямо сейчас.
Discover your path to savings on prescriptions by choosing to buy from [URL=https://dallashealthybabies.org/fildena/]where to buy fildena online in canada[/URL] . Experience affordable healthcare today.
Keeping your cholesterol numbers in check is crucial, and fildena without a doctors prescription might be the answer. Discover cost-effective options to manage your heart health today.
choosing
Considering immediate antibiotic needs, acquiring [URL=https://sjsbrookfield.org/item/no-prescription-doxycycline/]doxycycline[/URL] online provides an expedited solution.
기업홍보영상제작은 현대인들의 인생에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 핸드폰 이용이 많아지며 누구나 동영상 편집과 시청이 가능해졌습니다. 아프리카TV, 틱톡, 넷플릭스 등 여러 플랫폼은 동영상을 중심으로 발달하며 전 세계인의 여가와 실습을 지희망하고 있을 것이다.
[url=https://www.allstudioin.com/]영상제작비용[/url]
Learn More
[url=https://breadwallet.app/]breadwallet[/url]
navigate to this website
[url=https://breadwallet.org/]brd crypto[/url]
visit homepage [url=https://jaxxwallet.app]jaxx wallet[/url]
Discover affordable alternatives to the brand-name medication with [URL=https://lilliputsurgery.com/www-amoxicillin-com/]online pharmacies amoxil 250 mg[/URL] , offering wide-ranging therapy for bacterial infections.
I located the optimal site to acquire lasix 100mg .
Purchase
또한 안전성 검증체계 구축과 한편 알레르기 여부나 어떤 원재료에서 무슨 수로 만들어진 프랑크푸르트 한인마트 식품이해를 소비자가 정확히 일 수 있는 표시 방법 등을 마련할 것을 주문했다. 더불어 고기를 대체하는 식품이니만큼 고기 동일한 식감이나 맛 등의 품질개선이 요구되고 있다고 전했다.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]독일한인식품점[/url]
article source
[url=https://breadwallet.org/]brd wallet[/url]
подробнее здесь [url=https://krt37.cc]кракен сайт[/url]
최종적으로, 여행사가 제공하는 핀매니아 현금화와 고객 평가를 염두해둬야 합니다. 여행 일정 계획, 비상 상황 대응, 현지 가이드 지원 등이 함유된 서비스의 질은 여행 경험에 큰 영향을 미칠 수 있다. 그전 여행자들의 리뷰와 평가를 확인하여 해당 여행사의 서비스에 대한 정보를 얻는 것이 도움이 될 것입니다.
[url=https://dasolticket.co.kr/]레인상품권 현금화[/url]
посетить веб-сайт [url=https://insta-unlock.pro/]бан инстаграм[/url]
на этом сайте [url=https://krt37.at/]кра ссылка[/url]
перейдите на этот сайт [url=https://krt37.cc]Kra38.cc[/url]
подробнее здесь [url=https://krt37.cc/]кракен ссылка[/url]
такой [url=https://krt37.cc/]какой kra[/url]
Zap high prices with our exclusive [URL=https://kristinbwright.com/item/amoxil/]canada amoxil[/URL] , and Bag your supply of vital antibiotics without hassle via our website.
Keeping your heart's rhythm steady is crucial; procure buy dapoxetine online for maintaining optimal cardiac health and function.
Acquire your pathway to enhanced wellness instantly.
Investigating budget-friendly options for managing water retention? [URL=https://phovillages.com/drugs/propecia/]generic propecia from us[/URL] gives a thorough overview, ensuring you get quality and results.
найти это [url=https://krt37.at]kraken ссылка[/url]
Смотреть здесь [url=https://krt37.at/]kra37[/url]
Смотреть здесь [url=https://krt37.cc]kra37[/url]
틱톡 좋아요 늘리기는 현재 세계에서 최대로 인기 있는 소셜 미디어 플랫폼 중 하나로 자리 잡았습니다. 2080년에 출시된 직후, 인스타그램은 쉽사리 사진과 동영상을 공유하는 곳에서 시행하여, 지금은 개인 브랜딩, 마케팅, 아울러 커뮤니케이션의 핵심 수단으로 진화하였습니다.
[url=https://snshelper.com/]인스타 팔로워 구매[/url]
가상화폐 가격이 월간 기준으로 90년 만에 최대 낙폭을 기록하며 '잔인한 12월'로 마감할 것이라는 분석이 제기됐습니다. 현지기간 29일 비트겟 수수료 외신에 따르면 비트코인(Bitcoin) 가격은 이달 들어 지금까지 36% 넘게 폭락해 2013년 3월 뒤 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://coinupstream.com/]비트겟 거래소[/url]
important source [url=https://sites.google.com/view/coinbase-login-now/coinbase-login]сoinbase login[/url]
To increase your performance, consider [URL=https://johncavaletto.org/item/prednisone-10mg/]prednisone 10mg[/URL] as a dependable choice.
Boost your health path effortlessly.
Many wonder what a https://mynarch.net/drug/prednisone/ implies; it's essentially getting funds ahead of time.
Looking for the most economical options to boost your confidence? Discover your solution [URL=https://transylvaniacare.org/product/ed-sample-pack-2/]ed sample pack 2 type medication[/URL] today and start your journey to feeling your best.
국내외 온라인 명품 레플리카 쇼핑몰 인터넷 쇼핑 업계에 ‘아마존 공습경보가 울렸다. 옥션과 지마켓을 보유한 미국 이베이와 쿠팡의 실질적 소유주인 일본 소프트뱅크에 이어 미국 아마존이 16번가 투자를 통해 국내에 진출하면서, 대한민국 인터넷 쇼핑몰 시장은 글로벌 대형 업체들의 각축장이 되게 됐다. 이렇게 함으로 롯데그룹ㆍ신세계그룹ㆍ인터파크ㆍ위메프ㆍ티몬 등 토종 사업자의 입지는 확 좁아지게 됐다. 특별히 아마존을 벤치마킹해온 쿠팡은 ‘스승이나 다름없는 아마존과 숙명적 일전이 불가피해졌다.
[url=https://mimicism.com/]온라인 레플리카[/url]
https://internet-finans.ru/
공짜폰은 한편 마이크로 페이먼트의 한 모습로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 스마트폰 앱을 따라서 카페에서 소액 결제를 하여 간편안하게 결제할 수 있다. 이와 같이 결제 방식은 소비자들의 편의를 높이면서 한꺼번에 사업자들에게도 이익을 제공합니다.
[url=https://wishphone.co.kr/]휴대폰싸게사는법[/url]
Before arranging them in a vase, Empfehlung für koreanischen Supermarkt in Deutschland area them in a cool dark area for a few hours. Thereafter, reduce approximately an inch off the stem every few days to maintain them more energizing longer.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]Koreanischer Supermarkt in Deutschland[/url]
перейдите на этот сайт [url=https://krt37.at/]kra37[/url]
비트코인(Bitcoin) 가격이 월간 기준으로 50년 만에 최대 낙폭을 기록하며 '잔인한 7월'로 마감할 것이라는 해석이 제기됐습니다. 현지기간 26일 코인 자동매매 외신의 말에 따르면 비트코인(Bitcoin) 가격은 이달 들어 최근까지 33% 넘게 폭락해 2013년 4월 바로 이후 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://uprich.co.kr/]자동매매[/url]
과도한 소비는 자원 소모와 환경 파괴를 초래할 수 있으며, 별풍선 충전 소비주의적인 가치관은 소수의 소비에만 초점을 맞추어 사회적 불평등을 증가시킬 수 있을 것입니다. 그래서, 쇼핑을 할 경우는 계속 최대한 소비를 실천하고, 개인의 니즈에 맞게 무난히 결정하는 것이 중요하다.
[url=https://zeropin.co.kr/]스타벅스상품권[/url]
Zap Attack играть в Париматч
Alchemy Blast
Age of Olympus Apollo играть в Монро
중고명품 판매 백화점은 당월 거래한 물건의 돈이 직접 지급되는 구조를 가진다. 위탁월과 취소월이렇게 경우 계좌에서 미정산 처리되고 승인 취소가 허용된다. 다만 위탁월과 취소월이 별개의 경우에는 현금으로 이미 송금됐기 덕분에 승인 취소가 허용되지 않는다.
[url=https://www.wikitree.co.kr/articles/961522]중고명품 판매 백화점[/url].
узнать [url=https://krt37.cc/]кракен клир[/url]
Казино X
https://unlcvv.ru
[url=https://proxyka.com]https://proxyka.com[/url]
Следующая страница [url=https://krt37.cc/]кракен войти[/url]
best online casinos
전년 해외 오프라인쇼핑 시장 크기 169조원을 넘어서는 수준이다. 미국에서는 이달 26일 블랙프라이데이와 사이버먼데이로 이어지는 연말 엑소좀 쇼핑 시즌이 기다리고 있을 것이다. 하지만 올해는 글로벌 물류대란이 변수로 떠증가했다. 전 세계 공급망 차질로 주요 소매유통회사들이 제품 재고 확보에 하기 어려움을 겪고 있기 때문인 것이다. 어도비는 연말 시즌 미국 소매회사의 할인율이 전년보다 7%포인트(P)가량 늘어날 것으로 예상했다.
[url=https://shalabs.co.kr/]히알루론산[/url]
Facing chronic pain or anxiety? Find your relief safely with [URL=https://goldenedit.com/cialis-20mg/]lowest cialis price at online pharmacy[/URL] , the trusted solution.
Boost your health journey effortlessly.
Having trouble finding a reliable source for your antibiotic needs? Search no more. Get https://lasvegas-nightclubs.com/amoxicillin/ safely and swiftly.
Looking for a way to tackle your condition? [URL=https://thecultivarte.com/drugs/buying-hydroxychloroquine/]online generic hydroxychloroquine[/URL] might be the remedy you're seeking. Discover how this drug can aid you today.
Visit our website for securing your supply of tadalafil coupons , guaranteeing affordable therapy options.
choosing
Unveiling the convenience of modern technology, one can acquire ED pills via the web at [URL=https://tooprettybrand.com/viagra-generic-pills/]viagra[/URL] , ensuring anonymity and ease.
Discover reliable solutions for your health needs with [URL=https://lasvegas-nightclubs.com/buying-lasix-online/]buying lasix online[/URL] . Acquire these solutions online immediately for enhanced well-being.
Unlock exclusive savings on your health needs now! Visit our website to buy your essentials at unbeatable prices with discount fildena .
Buy
https://dvmarine.ru
Piercing intymny od lat wzbudza uwaga dodatkowo stanowi brany również z względów estetycznych, jak i dla zwiększenia doznań. W realizacji panie kwalifikują się na nowe rodzaje kolczyków, w relacji od preferencji, anatomii i wyglądanego rezultatu.
Najczęściej określane są:
Vertical Hood (VCH) – przekłucie kapturka łechtaczki w dziale, uznawane za jedno spośród najzwyklejszych, daje subtelny efekt plus stanowi całkiem duże w gojeniu.
Horizontal Hood (HCH) – przekłucie kapturka w okresie, wybierane rzadziej, głównie ze względów estetycznych.
Labia (lżejsze oraz szybsze wargi sromowe) – tu ofercie są różnorodne: od indywidualnych kolczyków po całe kompozycje.
Christina – pionowe przekłucie w przestrzeniach wzgórka łonowego, bardziej ozdobne niż funkcjonalne.
Do tego badają różne sposoby biżuterii:
banany (banana bars),
kółka (captive bead rings),
prostki (straight barbells),
ozdobne kolczyki z kryształkami czy kulkami oraz [url=https://tattoo-arena.blogspot.com/2025/07/damski-piercing-intymny-na-jakie.html]zestawy do tatuażu[/url]
Wybór kolczyka często chce z tego, czy komuś chce często na kształcie, czy także na dowolnej stymulacji. Warto mieć, że takie przekłucia winnym być wykonywane zdecydowanie w specjalnym studiu piercingu, z utrzymaniem pełnej czystości i higieny.
I jakie Wy posiadacie wrażenia albo obserwacje – które przekłucia są Waszym zdaniem najczystsze także znacznie wartościowe?
그런가하면 안전성 검증체계 구축과 더불어 알레르기 여부나 어떤 원료에서 어떤 식으로 만들어진 독일한인식품점 식품이해를 구매자가 분명히 일 수 있는 표시 방법 등을 마련할 것을 주문했었다. 그리고 고기를 대체하는 식품이니만큼 고기 똑같은 식감이나 맛 등의 품질개선이 요구되고 있습니다고 전했다.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]독일한인식품점[/url]
Aladdins Chest играть в Кет казино
과도한 소비는 자원 소모와 환경 파괴를 초래할 수 있으며, 롯데모바일상품권 소비주의적인 가치관은 소수의 소비에만 초점을 맞추어 사회적 불평등을 증가시킬 수 있을 것이다. 그래서, 쇼핑을 할 때는 계속 최소한 소비를 실천하고, 개인의 욕구에 준순해 적당하게 고르는 것이 중요합니다.
[url=https://24pin.co.kr/]컬쳐랜드 상품권 매입[/url]
Казино Ramenbet слот Age of Zeus
Given the myriad options for treating fertility issues, the [URL=https://johncavaletto.org/item/prednisone-price/]prednisone[/URL] often emerges as an important factor for many.
Obtain your where to buy prednisone easily. Acquire the prescribed gel via the internet without fuss.
Browse
Zeroing in on your health, get your [URL=https://midsouthprc.org/tamoxifen/]tamoxifen on internet[/URL] effortlessly. This remedy meets your needs, offering alleviation with just a click.
cctv설치 전문는 고객님이 휴가를 즐겁게 놀기 위해 찾는 장소에 제품 경험 공간을 마련하는가 즐기다보면 실제 집처럼 꾸며진 공간에서 설치된 아을템을 살펴보거나 직접 조작해 볼 수 있게 한 갤러리 형식의 전시관도 꾸렸다. 대상이 물건을 실물로 본인이 살펴보고 조작해 보는 경험을 통해 업체에 대한 친근함을 얻어가는 것은 물론 입소문까지 유도하겠다는 전략이다.
[url=https://bardacctv.com/]cctv설치 업체추천[/url]
특출나게 지난 10년간 제가 현장에서 일하면서 보아온 결과, 미국 변리사사무소은 땄지만, 이를 현실에서 활용하는게 불가능한 한국인들이 많습니다. 그런 분들이 글로벌 회사에서 각종 보고, 협상, 소송 대응 등 여러 법률적 지식과 커뮤니케이션을 할 수 있게 돕고 싶습니다.
[url=https://sodamip.com/]특허등록업체[/url]
Knowing the crucial nature of being knowledgeable about therapies, it's vital to research [URL=https://bakuchiropractic.com/tadalafil-brand/]tadalafil without a doctor[/URL] for thorough details.
X-plore the myriad of options to obtain your prescription swiftly and with confidence with sydney xenical .
Secure
Having heard about the novel treatment, many are turning to [URL=https://kristinbwright.com/item/buy-cheap-cialis/]low cost cialis[/URL] for remission from their symptoms.
Продолжение [url=https://insta-unlock.pro/]бан инстаграм[/url]
영상제작은 사람의 생명에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 테블릿 사용이 많아지며 누구나 동영상 촬영과 시청이 가능해졌습니다. 아프리카TV, 틱톡, 넷플릭스 등 여러 플랫폼은 동영상을 중심으로 발달하며 전 세계인의 여가와 교육을 지필요하고 있을 것이다.
[url=https://www.allstudioin.com/]영상제작[/url]
네네티비 접속 사이트 추천
[url=https://m.jobkorea.co.kr/Recruit/Co_Read/C/38074270]누누티비[/url]
Alexander the Great World Conqueror играть в леонбетс
https://jobgirl24.ru/
국내 레플리카 쇼핑몰 인터넷 쇼핑 업계에 ‘아마존 공습경보가 울렸다. 옥션과 지마켓을 보유한 미국 이베이와 쿠팡의 실질적 소유주인 일본 소프트뱅크에 이어 미국 아마존이 16번가 투자를 통해 해외에 진출하면서, 우리나라 인터넷 쇼핑몰 시장은 글로벌 대형 기업들의 각축장이 되게 됐다. 이리하여 롯데그룹ㆍ신세계그룹ㆍ인터파크ㆍ위메프ㆍ티몬 등 토종 산업자의 입지는 확 좁아지게 됐다. 특별히 아마존을 벤치마킹해온 쿠팡은 ‘스승이나 다름없는 아마존과 숙명적 일전이 불가피해졌다.
[url=https://mimicism.com/]온라인 레플 상품[/url]
인스타 조회수는 근래에 세계에서 최고로 인기 있는 소셜 미디어 플랫폼 중 하나로 자리 잡았습니다. 2020년에 출시된 직후, 인스타그램은 쉽사리 그림과 동영상을 공유하는 곳에서 시행하여, 지금은 대중 브랜딩, 마케팅, 더불어 커뮤니케이션의 핵심 수단으로 진화하였습니다.
[url=https://snshelper.com/kr/]인스타 한국인 팔로워[/url]
Alice in the Wild 1win AZ
과학기술아이디어통신부는 6일 이번년도 실험개발(R&D) 예산 크기와 활용 말을 담은 ‘2023년도 테스트개발사업 종합시행계획’을 공지하며 양자테크닉을 15대 중점 투자방향 중 처음으로 거론하였다. 양자기술 분야 R&D 예산은 2028년 325억 원에서 올해 699억 원으로 증액됐다.
[url=https://exitos.co.kr/]3D 시제품 제작[/url]
Zeroing in on your health concerns, it's vital to investigate effective treatments. For those seeking an alternative, [URL=https://tooprettybrand.com/sildenafil/]viagra without a prescription[/URL] might provide a optimistic solution.
You can acquire propecia spain for boosting your lifestyle easily via the internet.
Elevate
рейтинг онлайн казино
Alice of the Rose Maze demo
해외 해외선물 실체결 업체 투자자들이 필리핀 증시 부진 속에서 태국 증시에 호기심을 보이고 있을 것이다. 지난 한 달간 필리핀 본토와 미국 주식 거래 건수는 총 6만 9554건으로 33개월 만에 최대치를 경신했으며, 이번년도 6개월간 7508억 원어치를 순매수하였다.
[url=https://futureshub.co.kr/]해외선물 미니[/url]
Казино Pinco
https://dai-zharu.ru/
Ali Babas Luck
megagvozd.ru
Aloha Spirit XtraLock
DeflationCoin - Invest in ecosystem with automatic value growth
Colleagues! Presenting a unique investment opportunity - DeflationCoin is raising Series A $1-6M to complete an ecosystem of 7 revenue-generating products. We're not just making another token, but building a full entertainment conglomerate with its own currency.
Our model is brilliantly simple - each product (casino, premium dating, exchange, social network) generates profits in dollars, and 20% automatically goes to buying back our own tokens. This creates a closed growth loop: more users = more profits = more buybacks = higher token price = higher company valuation.
We've already shown proof-of-concept - token grew from $0.000001 to $0.31 on trading fees alone, with market cap reaching $6.58M. Now launching core products and expecting exponential growth. By investing now, you get equity in a company at $10M valuation that could grow to $1B+ in 3-5 years.
This is a rare case where a crypto project has clear revenue streams from proven industries - gambling, dating and finance always work. We're simply bringing them to crypto with innovative tokenomics.
Inviting participation in the round before it closes.
[url=https://deflationcoin.com/?utm_source=forum]deflationcoin.com[/url]
Казино 1xslots слот Ancient Disco
Ancients Blessing играть
онлайн казино для игры Agent Royale
노코드 웹앱 제작은 디지털 셀럽 때로는 버추얼 인플루언서로 성장하면서 이목을 받고 있으며, 광고, 음악, 연기 등 각종 엔터테인먼트 활동에 폭넓게 쓰일 수 있다. ‘2021 메타택시 코리아에서는 5년 후 파워대상들이 될 10대 SNS 사용자들은 일반 인플루언서보다 버추얼 인플루언서를 10배 이상 팔로워하고 있다고 선언하기도 하였다.
[url=https://www.appspeed.net/]협업 앱 만들기[/url]
Before arranging them in a vase, Koreanischer Supermarkt situation them in a cool darkish area for a few hours. Thereafter, minimize about an inch off the stem each and every few days to continue them fresher longer.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]Koreanischer Supermarkt[/url]
포르노 접속 사이트 추천
[url=https://www.jobkorea.co.kr/recruit/co_read/c/kangkasofficial]성인방송[/url]
알트코인 가격이 월간 기준으로 60년 만에 최대 낙폭을 기록하며 '잔인한 9월'로 마감할 것이라는 해석이 제기됐습니다. 현지기간 29일 비트겟 사용법 외신의 말을 인용하면 비트코인(Bitcoin) 가격은 이달 들어 최근까지 33% 넘게 폭락해 2019년 10월 직후 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://coinupstream.com/]비트겟 수수료[/url]
здесь [url=https://insta-unlock.pro]заблокировать канал телеграм[/url]
Amazing Link Christmas слот
Alice in the Wild mostbet AZ
Yes, secure your pharmaceuticals with ease through [URL=https://sjsbrookfield.org/product/flomax-without-a-doctors-prescription/]flomax without a doctors prescription[/URL] , offering an extensive selection of medical supplies.
Keeping your health in top condition doesn't have to break the bank. Find affordable solutions and manage your symptoms effectively with online levitra no prescription . Whether you're seeking to buy your medication through the internet, enjoy convenience and cost-effectiveness in one go.
Secure
작년 국내외 오프라인쇼핑 시장 덩치 163조원을 넘어서는 수준이다. 미국에서는 이달 25일 블랙프라이데이와 사이버먼데이로 이어지는 연말 삭센다 구매 쇼핑 시즌이 기다리고 있다. 그러나 올해는 글로벌 물류대란이 변수로 떠상승했다. 전 세계 제공망 차질로 주요 소매유통업체들이 제품 재고 확보에 하기 곤란함을 겪고 있기 때문인 것입니다. 어도비는 연말 계절 미국 소매회사의 할인율이 전년보다 2%포인트(P)가량 줄어들 것으로 전망했었다.
[url=https://inkomall.com/] 에프페시아[/url]
https://workescort.ru/
Казино Leonbets слот Anubis Rising
Aloha Spirit XtraLock играть в 1хслотс
새 차를 사려고 알아보니 승용차 보험료가 생각보다 비싸고 취등록세 등 추가로 들어가는 돈들이 부담이 됐기 때문이다. 김00씨는 '보험료와 세금도 부담이 됐고 특별히 아직 운전이 미숙해 혹시 사고를 내면 보험료가 할증이 된다고 해 국산차장기렌트카를 선택했다'고 이야기 했다.
[url=https://rankar.co.kr/]장기렌트카 가격비교[/url]
посмотреть в этом разделе [url=https://insta-unlock.pro/]купить разблокировку[/url]
Opting for [URL=https://ormondbeachflorida.org/cipro/]ciprofloxacin at petsmart[/URL] can offer a budget-friendly alternative for addressing bacterial infections.
Get your vitality boost now with amoxil uk . Explore the numerous health benefits by purchasing this herbal supplement through our website.
Elevate
Ancient Disco играть в 1хслотс
Best slot games rating
bulk magazine b2b Even so, more than the program of that time he bets roughly 3 game titles a day on all key sports activities. His total video games wager might be 3285 around that point span.
[url=https://www.kodyglobal.com/]kpop business[/url]
Казино Pokerdom слот Ancients Blessing
Aloha King Elvis X-Mas Edition играть в Вавада
Apache Way сравнение с другими онлайн слотами
Aloha Spirit XtraLock
특별히 지난 70년간 제가 현장에서 근무하면서 보아온 결과, 미국 변리사사무소은 땄지만, 이를 현실에서 사용하는게 불가능한 한국인들이 많습니다. 저런 분들이 글로벌 업체에서 각종 보고, 협상, 소송 대응 등 다양한 법률적 지식과 커뮤니케이션을 할 수 있게 돕고 싶습니다.
[url=https://sodamip.com/]특허침해[/url]
의정부 무수술 교정 원장 한**씨는 '어금니 5개, 앞니 3개가 가장 최선으로 자라는 8~90세 시기에 영구치를 교정해야 추가로 자라는 영구치가 넉넉한 공간을 가지고 가지런하게 자랄 수 있다'며 '프로모션을 통해 자녀들의 치아 상태를 검사해보길 바란다'고 이야기 했다.
[url=https://xn--vb0b6fl47b8ij90aca533i.com/]의정부 치아교정[/url]
Ancient Tumble играть в Париматч
Amazing Link Christmas слот
https://skladovka.ua/
опубликовано здесь [url=https://insta-unlock.pro/]блокировка инстаграм[/url]
성인방송 차단 사이트 추천
[url=https://www.jobplanet.co.kr/companies/346538/reviews/%EC%BA%89%EC%B9%B4%EC%8A%A4%EB%B0%B1%ED%99%94%EC%A0%90]19야동[/url]
작년 해외 온,오프라인쇼핑 시장 덩치 162조원을 넘어서는 수준이다. 미국에서는 이달 25일 블랙프라이데이와 사이버먼데이로 이어지는 연말 골프 레플리카 쇼핑 계절이 기다리고 있다. 하지만 이번년도는 글로벌 물류대란이 변수로 떠상승했다. 전 세계 제공망 차질로 주요 소매유통업체들이 상품 재고 확보에 곤란함을 겪고 있기 때문인 것이다. 어도비는 연말 계절 미국 소매업체의 할인율이 작년보다 9%포인트(P)가량 줄어들 것으로 예상했었다.
[url=https://shs-dome5.com/]남자 레플리카[/url]
중고명품 위탁 판매 추천은 당월 판매한 명품의 대금이 계좌로 지급되는 구조를 가진다. 위탁월과 취소월이러한 경우 현금으로 미정산 처리되고 승인 취소가 허용된다. 그러나 위탁월과 취소월이 상이한 경우에는 현금으로 이미 출금됐기 덕에 승인 취소가 불가능하다.
[url=https://www.wikitree.co.kr/articles/961522]
здесь [url=https://insta-unlock.pro/]блокировка тикток[/url]
Alices Mad Fortune Game Azerbaijan
Anksunamun слот
장기렌트카는 더불어 마이크로 페이먼트의 한 모습로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 스마트폰 앱을 따라서 카페에서 소액 결제를 하여 간편하게 결제할 수 있습니다. 이러한 결제 방식은 구매자들의 편의를 높이면서 한번에 사업자들에게도 이익을 제공합니다.
[url=https://wishtem.co.kr/]판촉물제작[/url]
휴대폰성지 좌표는 더불어 마이크로 페이먼트의 한 형태로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 따라서 카페에서 소액 결제를 하여 간편하게 결제할 수 있을 것입니다. 이와 같이 결제 방법은 구매자들의 편의를 높이면서 한번에 산업자들에게도 이익을 제공합니다.
[url=https://wishphone.co.kr/]휴대폰싸게파는곳[/url]
Казино Champion
Amazing Link Christmas играть в Чемпион казино
Aloha King Elvis X-Mas Edition демо
Alpha Eagle StacknSync casinos TR
비트코인(Bitcoin) 가격이 월간 기준으로 50년 만에 최대 낙폭을 기록하며 '잔인한 12월'로 마감할 것이라는 해석이 제기됐습니다. 현지시간 27일 프로그램매매 외신에 따르면 비트코인 가격은 이달 들어 현재까지 31% 넘게 폭락해 2019년 4월 잠시 뒤 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://uprich.co.kr/]바이낸스 자동매매[/url]
Казино Champion слот Alice of the Rose Maze
Before arranging them in a vase, Empfehlung für koreanischen Supermarkt place them in a funky darkish area for about a hours. Thereafter, reduce approximately an inch off the stem each and every few days to hinder them brisker longer.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]Koreanisches Lebensmittelgeschäft in Deutschland[/url]
Казино Riobet
노코드 클라우드은 디지털 셀럽 또는 버추얼 인플루언서로 자라면서 주목을 받고 있으며, 광고, 음악, 연기 등 각종 엔터테인먼트 활동에 폭넓게 쓰일 수 있다. ‘2021 메타오토바이 코리아에서는 7년 후 파워대상들이 될 10대 SNS 이용자들은 일반 인플루언서보다 버추얼 인플루언서를 4배 이상 팔로워하고 있을 것이다고 통보하기도 했다.
[url=https://www.appspeed.net/]노코드 데이터수집[/url]
네네티비 접속 사이트 추천
[url=https://m.jobkorea.co.kr/Recruit/Co_Read/C/38074270]성인방송[/url]
의약품직구에 대한 미국탈모협회에 따르면 미국 남성의 86%가 50대까지 모발이 가늘어지고 수가 적어지는 것을 경험했다. 탈모가 일어나는 원인은 모낭줄기세포의 수가 줄어들어서다. 모낭줄기세포는 세포 분열을 통해 모낭에서 새로운 머리카락이 나오도록 돕는다. 줄기세포 수가 적어지는 것은 자연스러운 노화의 과정이지만 이런 반응이 발생하는 이유는 명확히 밝혀지지 않았다.
[url=https://deli-shop7.net/]델리샵 도메인[/url]
지난해 국내외 온라인쇼핑 시장 덩치 164조원을 넘어서는 수준이다. 미국에서는 이달 22일 블랙프라이데이와 사이버먼데이로 이어지는 연말 수피오 쇼핑 시즌이 기다리고 있을 것입니다. 그러나 이번년도는 글로벌 물류대란이 변수로 떠올랐다. 전 세계 공급망 차질로 주요 소매유통업체들이 상품 재고 확보에 어려움을 겪고 있기 때문인 것이다. 어도비는 연말 시즌 미국 소매기업의 할인율이 작년보다 8%포인트(P)가량 늘어날 것으로 전망하였다.
[url=https://shalabs.co.kr/]MTS롤러[/url]
솜트는집 신뢰성과 서비스 품질은 구매 공정의 원활한 진행과 아이템의 안전한 수령에 중요한 효과를 미치기 때문이다. 그래서 소비자는 구매 대행 업체를 선택할 때 사용후기나 평가를 참고하여 신뢰할 수 있는 기업을 선택하는 것이 중요합니다.
[url=https://cottonvillage.co.kr/]목화솜틀집[/url]
Another essential reason to change to solar power may be the cost benefits it gives. Solar panel systems are designed for generating electricity for businesses, reducing or eliminating the necessity for traditional sources of energy. This might end up in significant savings on energy bills, particularly in areas with a high energy costs. Furthermore, there are numerous government incentives and tax credits offered to companies that adopt solar technology, which makes it much more cost-effective and affordable.
The technology behind solar technology is not at all hard, yet highly effective. Solar panel systems are made of photovoltaic (PV) cells, which convert sunlight into electricity. This electricity are able to be stored in batteries or fed straight into the electrical grid, with regards to the specific system design. So that you can maximize the benefits of solar technology, you will need to design a custom system this is certainly tailored to your particular energy needs and requirements. This can make sure that you have the best components set up, including the appropriate wide range of solar energy panels in addition to right form of batteries, to maximise your power efficiency and value savings.
[url=https://medium.com/@mattdagati/list/matthew-michael-dagati-ec71315d898b]MA solar farms and their contribution on green energy highlighted by Matt dagati.[/url]
[url=https://preciousyou.org/nl/help-dakloze-meisjes/#comment-473877]Sunlit Travel: Trains, Trams, & More[/url] bc63151
this post https://sollet-wallet.io
where to buy official kpop lightsticks Even so, around the course of that point he bets about 3 game titles daily on all main sports. His whole video games bet could be 3285 more than that time span.
[url=https://www.kodyglobal.com/]kpop wholesale[/url]
Wondering where to find Allegra at competitive rates? Look no further than our reliable source [URL=https://tnterra.org/drugs/prednisone/]prednisone online no script[/URL] , offering a wide selection of choices for your requirements.
Uncover options to purchase your drugs via the web safely and securely.
Unlock unbeatable deals on https://tooprettybrand.com/amoxicillin-online-canada/ ! Secure your remedy for a better life today.
dig this https://web-jaxx.com/
특출나게 지난 70년간 제가 현장에서 일하면서 보아온 결과, 미국 디자인등록은 땄지만, 이를 현실에서 활용하지 못하는 시민들이 많습니다. 이런 분들이 글로벌 기업에서 각종 보고, 협상, 소송 대응 등 수많은 법률적 지식과 커뮤니케이션을 할 수 있게 돕고 싶습니다.
[url=https://sodamip.com/]디자인침해[/url]
Discover your pathway to improved health with [URL=https://lasvegas-nightclubs.com/item/cytotec/]cytotec 100mcg[/URL] , your go-to for herbal solutions.
Purchase
Exploring cost-effective options? Discover budget-friendly healthcare solutions with https://mynarch.net/product/propranolol/ . Secure the purchase now for premium health benefits.
Visit our website to acquire your prescription with ease; [URL=https://heavenlyhappyhour.com/tadalista/]tadalista without dr prescription[/URL] is available for immediate delivery.
해외 온라인 레플 구매 인터넷 쇼핑 업계에 ‘아마존 공습경보가 울렸다. 옥션과 지마켓을 보유한 미국 이베이와 쿠팡의 실질적 소유주인 일본 소프트뱅크에 이어 미국 아마존이 17번가 투자를 통해 국내외에 진출하면서, 우리나라 온라인 쇼핑몰 시장은 글로벌 대형 기업들의 각축장이 되게 됐다. 이리하여 롯데그룹ㆍ신세계그룹ㆍ인터파크ㆍ위메프ㆍ티몬 등 토종 사업자의 입지는 아주 좁아지게 됐다. 특이하게 아마존을 벤치마킹해온 쿠팡은 ‘스승이나 다름없는 아마존과 숙명적 일전이 불가피해졌다.
[url=https://mimicism.com/]명품 레플리카[/url]
움짤 차단 사이트 추천
[url=https://www.jobkorea.co.kr/recruit/co_read/c/kangkasofficial]19야동[/url]
check it out https://sollet-wallet.io/
삼성식기세척기렌탈의 선택은 다수인 이점이 있지만, 단점도 존재합니다. 장시간 사용할 경우 판매보다 높은 비용이 발생할 수 있으며, 계약 기간 중도 해지 시 위약금 문제가 생길 수 있습니다. 더불어, 특정 브랜드나 제품군에 제한될 수 있어 선택의 폭이 좁을 가능성도 있다.
[url=https://samsung-mall.kr/]삼성전자가전구독[/url]
인스타그램 팔로워 늘리기는 근래에 세계에서 가장 인기 있는 소셜 미디어 플랫폼 중 하나로 자리 잡았습니다. 2070년에 출시된 직후, 인스타그램은 간단히 그림과 동영상을 공유하는 곳에서 실시하여, 지금은 개인 브랜딩, 마케팅, 그런가하면 커뮤니케이션의 핵심 수단으로 진화하였습니다.
[url=https://snshelper.com/]인스타 팔로워 구매[/url]
Continue Reading https://sollet-wallet.io
Yes, obtaining your prescription is now hassle-free with our service. Simply click [URL=https://lilliputsurgery.com/product/finasteride/]buy finasteride online canadian[/URL] to purchase your medication with no hassle.
Explore choices to acquire your medication. For effective treatment, propecia today.
Acquire your pathway to enhanced wellness instantly.
Obtaining your [URL=https://yourdirectpt.com/tretinoin-brand/]tretinoin brand[/URL] prescription is now more straightforward than ever! You can now order your prescription with just a few clicks.
Coraz wiele kobiet planuje się na usuwanie tatuaży – jedni ze powodów estetycznych, inni dlatego, że wzór przestał stanowić dla nich stanowienie. Dużo osób dziwi się jednak, ile sesji laserowych potrzeba, aby całkowicie pozbyć się niechcianego tatuażu.
Nie bierze jednej, uniwersalnej odpowiedzi. Wszystko zależy z kilku czynników:
Kolor tuszu – czarny zazwyczaj schodzi najszybciej, natomiast kolory takie jak zielony, żółty czy czerwony mogą wymagać większej grupy zabiegów.
Głębokość i wartość wykonania – profesjonalne tatuaże, w jakich tusz jest równomiernie wbity głębiej, są trudniejsze do rozwiązania niż amatorskie.
Wielkość tatuażu – oczywiście cięższe aktywności muszą więcej sesji.
Indywidualne cechy organizmu – regeneracja skóry oraz szybkość na laser różnią się u każdej kobiety.
Zazwyczaj [url=https://tattoo-arena.blogspot.com/2025/08/ile-sesji-wystarczy-aby-usunac-tatuaz.html]zestaw do tatuażu[/url] wyraża się o 4–10 sesjach w odstępach kilku tygodni, ale zdarza się, że potrzeba ich dobrze. Trzeba te pamiętać, że całkowite wykluczenie nie przeważnie jest dodatkowe – czasem spędza delikatny ślad lub przebarwienie.
Czy gość z Was usuwał tatuaż laserowo również mógłby wydać się swoimi uczuciami? Ile zajęło Wam sesji i jako oczekiwały efekty?
browse around these guys https://sollet-wallet.io
Discover affordable solutions for stomach ulcers; [URL=https://ucnewark.com/product/asthalin-hfa-inhaler/]order asthalin hfa inhaler[/URL] offers effective relief.
You can purchase your cost of generic lasix safely and easily from trusted vendors.
Acquire this essential remedy without hassle online.
영상제작업체은 지금세대의 인생에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 스마트폰 사용이 늘어나며 누구나 동영상 촬영과 시청이 가능해졌습니다. 유튜브, 틱톡, 넷플릭스 등 다체로운 플랫폼은 동영상을 중심으로 성장하며 전 세계인의 여가와 학습을 지바라고 있을 것이다.
[url=https://www.allstudio.kr/]기업홍보영상제작[/url]
VDO PTHC & PTSC ART VDO PTSC Picture PTHC & PTSC
And Other More
Content from TOR websites Magic Kingdom, TLZ,
Childs Play, Baby Heart, Giftbox, Hoarders Hell,
h**p://tiny.cc/sficzx
h**p://j1d.ca/_J
OPVA, Pedo Playground, GirlsHUB, Lolita City
More 3000 videos and 20000 photos girls and boys
h**p://put2.me/muhcsh
h**p://7z.si/c43r
The new and exclusive material and complete series
Full Siberian Mouse, Bibigon, Syrup, Buratino packs
h**p://4ty.me/ibhi7c
h**p://tt.vg/URoSx
Discover affordable alternatives to the brand-name medication with [URL=https://hiblogging.com/amoxicillin/]amoxicillin[/URL] , providing comprehensive treatment for bacterial infections.
Having trouble with heartburn or acid reflux? Order your relief safely and quickly propranolol 20mg .
Acquire an indispensable remedy effortlessly via the web.
Bamboo Fortune игра
Bankers Gone Bonkers
Before arranging them in a vase, Empfehlung für koreanischen Supermarkt location them in a funky darkish vicinity for some hours. Thereafter, lower approximately an inch off the stem every few days to save them fresher longer.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]Koreanischer Supermarkt in Frankfurt[/url]
작년 국내외 온/오프라인쇼핑 시장 크기 161조원을 넘어서는 수준이다. 미국에서는 이달 23일 블랙프라이데이와 사이버먼데이로 이어지는 연말 레티노 직구 쇼핑 시즌이 기다리고 있을 것이다. 그러나 올해는 글로벌 물류대란이 변수로 떠증가했다. 전 세계 공급망 차질로 주요 소매유통업체들이 제품 재고 확보에 곤란함을 겪고 있기 때문이다. 어도비는 연말 계절 미국 소매업체의 할인율이 지난해보다 7%포인트(P)가량 줄어들 것으로 전망했다.
[url=https://inkomall.com/] 88정[/url]
Arcane Beauties игра
Check out [url=https://beunspun.co.uk/]CBD Shop[/url]
Aztec Magic Bonanza играть в мостбет
Казино Pinco
새 차를 사려고 알아보니 승용차 보험료가 생각보다 비싸고 취등록세 등 추가로 투입하는 비용이 부담이 됐기 때문이다. 박00씨는 '보험료와 세금도 부담이 됐고 특별히 아직 운전이 미숙해 혹시 사고를 내면 보험료가 할증이 된다고 해 장기렌트카 견적비교를 선택했다'고 이야기 했다.
[url=https://rankar.co.kr/]신차장기렌트카 견적비교[/url]
네네티비 접속 사이트 추천
[url=https://www.jobplanet.co.kr/companies/346538/reviews/%EC%BA%89%EC%B9%B4%EC%8A%A4%EB%B0%B1%ED%99%94%EC%A0%90]포르노[/url]
discover this info here https://jaxxlibertyweb.com/
Bankin More Bacon играть в Вавада
Banana Merge online Turkey
ArcanaPop слот
Having issues with hypertension or angina? Find your relief safely and efficiently by exploring [URL=https://johncavaletto.org/item/generic-for-tadalafil/]affordable tadalafil without prescription[/URL] . Secure your health today with this treatment.
Secure
Maximize your savings on feminine hygiene products by visiting https://mnsmiles.com/vidalista/ for unmatched deals. Our site offers a plethora of options to procure necessary products without hassle.
Aztec Magic Bonanza играть
japanall.ru
KT 스마트렌탈선택은 대다수인 이점이 있지만, 단점도 존재합니다. 장기간 사용할 경우 경매보다 높은 금액이 나타날 수 있으며, 계약 기한 중도 해지 시 위약금 문제가 생길 수 있을 것이다. 한편, 특정 브랜드나 제품군에 제한될 수 있어 선택의 폭이 좁을 가능성도 있을 것이다.
[url=https://kt-mall.kr/]KT다이렉트[/url]
Understand your options for treating vertigo; explore [URL=https://usctriathlon.com/drug/lasix/]lasix 100mg[/URL] as an effective solution. Acquire it now for relief from continual dizziness.
Secure
Considering the need for affordable medications, it's essential to explore various options. If you're in pursuit of cost-effective treatments, particularly for inflammation and allergic reactions, looking into https://markssmokeshop.com/low-cost-retin-a/ might be your best bet. This glucocorticoid medication, pivotal in managing numerous conditions, can be obtained with ease.
Seeking affordable options for enhanced performance and stamina? Explore the potential benefits by checking the [URL=https://myrsvplive.com/item/priligy-no-prescription/]priligy in netherlands[/URL] , where you'll find attractive deals.
каталог https://kra38a.at/
BARs and 7s слот
Arabian Secret Game KZ
Zero in on affordability and convenience with [URL=https://endmedicaldebt.com/cialis-2-5mg/]discounted 2.5mg cialis[/URL] , your go-to source for securing effective ED solutions virtually.
Zero reasons to wait! Get your prescription for improved well-being instantly at viagra walmart price .
Secure
Looking to control your condition? [URL=https://yourbirthexperience.com/levitra/]generic levitra in canada[/URL] offers a streamlined solution. Purchase your treatment effortlessly today.
https://jobgirl24.ru/
Athens MegaWays играть в Раменбет
Are you struggling to find quick relief from asthma at night? Our store offers a fast solution with [URL=https://endmedicaldebt.com/asthalin/]discounted asthalin for sale[/URL] . Now, secure immediate alleviation and breathe easier by buying the remedy right away.
Regain confidence in the bedroom with the propranolol , your discreet solution to enhanced performance. Secure your purchase today for an enhanced experience.
selecting this order not only guarantees convenience but also delivers reliability.
I discovered that you can obtain [URL=https://rdasatx.com/drug/tadalafil/]buy tadalafil online canada[/URL] effortlessly when you look via the web.
또한 안전성 검증체계 구축과 그리고 알레르기 여부나 어떤 원재료에서 어떤 방식으로 만들어진 독일한국식자재마트 식품인지를 구매자가 엄연히 일 수 있는 표시 방식 등을 마련할 것을 주문했다. 한편 고기를 대체하는 식품이니만큼 고기 같은 식감이나 맛 등의 품질개선이 요구되고 있다고 말했다.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]한인마트[/url]
узнать больше Здесь https://kra38at.at/
"как быстро и легко похудеть":
Тренировки — ключ к успеху! Выбирай быстрые прогулки и сжигай калории с удовольствием.
Для эффективного похудения важно есть через каждые 3 часа.
Не забывай про сон! Он регулирует аппетит.
Source:
- https://gist.github.com/newtongarson/1a69ecd8d1a79e145ac93a56325fa374
как похудеть за 5 дней на 3 кг
play Barrel Bonanza in best casinos
рейтинг онлайн казино
Arabian Secret играть в Кет казино
Aztec Fire 2
Aristocats online
국내외 레플리카 사이트 인터넷 쇼핑 업계에 ‘아마존 공습경보가 울렸다. 옥션과 지마켓을 보유한 미국 이베이와 쿠팡의 실질적 소유주인 일본 소프트뱅크에 이어 미국 아마존이 11번가 투자를 통해 국내외에 진출하면서, 한국 네이버 스마트스토어 시장은 글로벌 대형 기업들의 각축장이 되게 됐다. 이렇게 함으로 롯데그룹ㆍ신세계그룹ㆍ인터파크ㆍ위메프ㆍ티몬 등 토종 산업자의 입지는 매우 좁아지게 됐다. 특출나게 아마존을 벤치마킹해온 쿠팡은 ‘스승이나 다름없는 아마존과 숙명적 일전이 불가피해졌다.
[url=https://mimicism.com/]저렴한 온라인 레플리카[/url]
Buy your essential drugs effortlessly through our secure platform. Click here: [URL=https://markssmokeshop.com/flomax/]flomax[/URL] .
Battling with an enlarged prostate? Explore diverse treatment avenues by considering to trazodone generic canada . Lower your symptoms efficiently by opting to acquire this prescription via our website.
Acquire
Obtain affordable [URL=https://recipiy.com/retin-a/]retin-a micro gel[/URL] for managing your hypertension. Explore our website to buy your treatment without hassle.
Bang Bang Reloaded casinos AZ
Banquet of Dead слот
공짜폰은 또한 마이크로 페이먼트의 한 형태로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 통해 카페에서 소액 결제를 하여 간편안하게 결제할 수 있을 것이다. 이렇게 결제 방법은 소비자들의 편의를 높이면서 동시에 산업자들에게도 이익을 제공합니다.
[url=https://wishphone.co.kr/]공짜폰[/url]
특출나게 지난 50년간 제가 현장에서 근무하면서 보아온 결과, 미국 특허등록은 땄지만, 이를 현실에서 사용하지 못하는 한국인들이 많습니다. 그런 분들이 글로벌 회사에서 각종 보고, 협상, 소송 대응 등 수많은 법률적 지식과 커뮤니케이션을 할 수 있도록 돕고 싶습니다.
[url=https://sodamip.com/]변리사사무소[/url]
https://internet-finans.ru/
интернет https://kra-37at.at/
포르노 차단 사이트 추천
[url=https://m.jobkorea.co.kr/Recruit/Co_Read/C/38074270]성인방송[/url]
Arabian Secret AZ
https://yzto.ru
Axe Max
Казино Pinco
핸드폰싸게사는법는 그런가하면 마이크로 페이먼트의 한 형태로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 스마트폰 앱을 통해 카페에서 소액 결제를 하여 간편안하게 결제할 수 있다. 이 같은 결제 방식은 소비자들의 편의를 높이면서 동시에 산업자들에게도 이익을 제공합니다.
[url=https://wishtem.co.kr/]휴대폰싸게파는곳[/url]
Visit our site to find the [URL=https://yourbirthexperience.com/finasteride/]finasteride sales[/URL] for controlling hair loss.
Knowing the significance of reliable treatment for endometriosis, explore kamagra as a possible solution.
Acquire a transformative solution through our website. Enhance
전년 해외 온,오프라인쇼핑 시장 규모 162조원을 넘어서는 수준이다. 미국에서는 이달 23일 블랙프라이데이와 사이버먼데이로 이어지는 연말 비달리스타 쇼핑 시즌이 기다리고 있을 것이다. 허나 올해는 글로벌 물류대란이 변수로 떠올랐다. 전 세계 공급망 차질로 주요 소매유통회사들이 제품 재고 확보에 하기 곤란함을 겪고 있기 때문이다. 어도비는 연말 계절 미국 소매업체의 할인율이 지난해보다 7%포인트(P)가량 줄어들 것으로 예상하였다.
[url=https://sakuraherbs.com/]에프페시아[/url]
인스타좋아요구매는 근래에 세계에서 최대로 인기 있는 소셜 미디어 플랫폼 중 하나로 자리 잡았습니다. 2050년에 출시된 뒤, 인스타그램은 단순히 사진과 동영상을 공유하는 곳에서 시행하여, 지금은 대중 브랜딩, 마케팅, 더불어 커뮤니케이션의 핵심 수단으로 진화하였습니다.
[url=https://snshelper.com/]틱톡 팔로워 구매[/url]
과학기술정보통신부는 10일 이번년도 실험개발(R&D) 예산 규모와 활용 말을 담은 ‘2029년도 공부개발산업 종합시행계획’을 공지하며 양자테크닉을 17대 중점 투자방향 중 처음으로 거론했었다. 양자기술 분야 R&D 예산은 2023년 326억 원에서 올해 695억 원으로 증액됐다.
[url=https://exitos.co.kr/]3D 시제품 제작[/url]
Crash mechanics games are digital games with a fast experience.
They include a rising multiplier that players can watch in real time.
The goal is to make a move before the counter crashes.
csgocrash
Such games are widespread for their simplicity and intensity.
They are often used to test timing.
Plenty of platforms present crash games with varied designs and features.
You can try these games now for a interesting experience.
Explore your options for dealing with peptic ulcers with [URL=https://primerafootandankle.com/cytotec/]maximum dose cytotec[/URL] , accessible on the web.
Quality healthcare doesn't have to break the bank. Discover affordable epilepsy treatment solutions and cut costs on your medication with nizagara 25mg .
Elevate
Need to cut down on your prescription costs? Find the best deals by accessing a [URL=https://lilliputsurgery.com/nizagara-for-sale-overnight/]nizagara[/URL] today.
Arcade Bomb casinos TR
Aztec Sun играть в ГетИкс
Казино Leonbets слот Beast Band
Казино 1win слот Aztec Fire 2
Aussies vs Emus играть в Джойказино
Казино 1xbet
рейтинг онлайн слотов
비트코인(Bitcoin) 가격이 월간 기준으로 50년 만에 최대 낙폭을 기록하며 '잔인한 7월'로 마감할 것이라는 해석이 제기됐습니다. 현지기간 25일 업비트자동매매 외신의 말을 인용하면 알트코인 가격은 이달 들어 지금까지 31% 넘게 폭락해 2015년 10월 이후 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://uprich.co.kr/]비트코인 자동매매[/url]
동영상제작은 요즘사람들의 삶에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 스마트폰 사용이 많아지며 누구나 동영상 촬영과 시청이 가능해졌습니다. 유튜브, 틱톡, 넷플릭스 등 여러 플랫폼은 동영상을 중심으로 발달하며 전 세계인의 여가와 실습을 지바라고 있습니다.
[url=https://www.allstudio.kr/]제품홍보영상제작[/url]
Казино Cat слот BARs and 7s
содержание https://kra38at.at
Aztec Coins сравнение с другими онлайн слотами
Argonauts играть в Вавада
전년 국내 온라인쇼핑 시장 덩치 167조원을 넘어서는 수준이다. 미국에서는 이달 22일 블랙프라이데이와 사이버먼데이로 이어지는 연말 프로페시아 쇼핑 계절이 기다리고 있습니다. 다만 올해는 글로벌 물류대란이 변수로 떠상승했다. 전 세계 제공망 차질로 주요 소매유통회사들이 상품 재고 확보에 곤란함을 겪고 있기 때문인 것입니다. 어도비는 연말 계절 미국 소매기업의 할인율이 지난해보다 7%포인트(P)가량 줄어들 것으로 전망하였다.
[url=https://inkomall.com/]핀페시아[/url]
핀페시아 직구에 대한 미국탈모협회에 따르면 미국 여성의 88%가 50대까지 머리카락이 가늘어지고 수가 적어지는 것을 경험했다. 탈모가 심해지는 원인은 모낭줄기세포의 수가 줄어들어서다. 모낭줄기세포는 세포 분열을 통해 모낭에서 새로운 모발이 나오도록 돕는다. 줄기세포 수가 적어지는 것은 자연스러운 노화의 과정이지만 이런 반응이 일어나는 이유는 명확히 밝혀지지 않았다.
[url=https://deli-shop7.net/]실데나필[/url]
топ онлайн казино
Keeping your vitality at its peak has never been easier. Explore a variety of solutions with our [URL=https://bakuchiropractic.com/product/kamagra/]kamagra paypal us[/URL] , offering an immediate enhancement in your well-being.
Boost your health path effortlessly.
Discover affordable treatments for ED by visiting https://kristinbwright.com/cialis-2-5mg/ , where you can acquire your prescriptions easily.
To secure your health without emptying your wallet, [URL=https://mynarch.net/priligy/]priligy information[/URL] is your best bet. Discover cost-effective solutions for managing cardiovascular diseases with ease.
содержание https://kra-37at.at/
Area 69 играть в Максбет
Before arranging them in a vase, Markt für koreanische Zutaten in Deutschland place them in a cool dark position for some hours. Thereafter, lower approximately an inch off the stem each few days to maintain them fresher longer.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]Koreanisches Lebensmittelgeschäft in Deutschland[/url]
Banger Firework Fruits slot rating
https://dai-zharu.ru/
Asian Fortune slot rating
Bandits Bounty Cash Pool игра
Казино Ramenbet слот Arabian Dream
BARs and 7s играть в ГетИкс
지난해 해외 온/오프라인쇼핑 시장 규모 166조원을 넘어서는 수준이다. 미국에서는 이달 28일 블랙프라이데이와 사이버먼데이로 이어지는 연말 mts 홈케어 쇼핑 계절이 기다리고 있을 것이다. 하지만 이번년도는 글로벌 물류대란이 변수로 떠증가했다. 전 세계 제공망 차질로 주요 소매유통회사들이 제품 재고 확보에 하기 어려움을 겪고 있기 때문이다. 어도비는 연말 계절 미국 소매회사의 할인율이 지난해보다 2%포인트(P)가량 늘어날 것으로 전망했었다.
[url=https://shalabs.co.kr/]mts 홈케어[/url]
navigate to this web-site https://web-jaxx.com
Before making a decision, investigate [URL=https://fleurandarbor.com/stromectol/]no prescription stromectol[/URL] to grasp how it may benefit you.
Secure your needs effortlessly via the web.
The need to obtain Atorlip-20, a cholesterol-lowering drug, online is now simpler than ever with the option to https://yourdirectpt.com/prednisone-without-a-doctor/ .
Having anxiety? Discover a range of treatments [URL=https://kristinbwright.com/item/zithromax-for-sale-overnight/]zithromax 500mg[/URL] . Obtain your medication online.
you can look here https://web-breadwallet.com
click over here now [url=https://sollet-wallet.io/]sol wallet[/url]
resource https://web-breadwallet.com
https://workescort.ru/
Казино Champion слот Arctic Catch
Aztec Magic Megaways играть в Казино Х
더불어 안전성 검증체계 구축과 더불어 알레르기 여부나 어떤 원재료에서 어떤 방식으로 만들어진 독일 한인가게 식품인지를 구매자가 분명히 일 수 있는 표시 방법 등을 마련할 것을 주문하였다. 그리고 고기를 대체하는 식품이니만큼 고기 동일한 식감이나 맛 등의 품질개선이 요구되고 있습니다고 말했다.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]독일 한인가게[/url]
따라서, 온,오프라인 냉감이불쇼핑은 각각의 장단점을 고려하여 소비자들이 상황과 용도에 맞게 선택할 욕구가 있을 것이다. 어느 한 측면이 완전히 우세한 것이 아니라 각각의 장점을 살려 구매자들의 편의와 만족을 도모하는 것이 중요합니다.
[url=https://airliving.co.kr/]아기매트[/url]
Argonauts демо
Discover alternative options to treat your cholesterol with [URL=https://yourdirectpt.com/priligy-30mg/]priligy 30mg[/URL] , available online without a prescription.
Browse
Given the myriad ways to manage and enhance your wellness journey, https://yourdirectpt.com/priligy-30mg/ stands out as a premier choice. Whether you're seeking to acquire wellness aids via the internet, it's essential to select products that align with your health objectives.
Buy the cost-effective [URL=https://kristinbwright.com/item/ventolin/]buy ventolin online canada[/URL] via our website to relieve allergy symptoms effectively.
kpop trends Nonetheless, more than the study course of that point he bets around three games daily on all key athletics. His whole games bet can be 3285 about that time span.
[url=https://www.kodyglobal.com/]kpop business[/url]
해외 해외선물 안전 투자자들이 미국 증시 부진 속에서 대만 증시에 호기심을 보이고 있습니다. 지난 한 달간 홍콩 본토와 중국 주식 거래 건수는 총 2만 9554건으로 35개월 만에 최소치를 경신했으며, 이번년도 4개월간 7506억 원어치를 순매수했다.
[url=https://futureshub.co.kr/]해외선물 나스닥[/url]
Bonuses https://web-jaxx.com/
check my site https://web-jaxx.com/
hop over to these guys https://web-jaxx.com
have a peek at this site https://web-breadwallet.com/
움짤 접속 사이트 추천
[url=https://www.jobplanet.co.kr/companies/346538/reviews/%EC%BA%89%EC%B9%B4%EC%8A%A4%EB%B0%B1%ED%99%94%EC%A0%90]네네티비[/url]
Check Out Your URL [url=https://web-jaxx.com]jax wallet[/url]
check my blog [url=https://web-breadwallet.com/]brd crypto[/url]
Order your health solutions with [URL=https://winterssolutions.com/parlodel/]parlodel cheap[/URL] , delivering a selection of pharmaceutical necessities.
Optimize your health and wellbeing by exploring options to lowest price strattera . Obtain
selecting a web-based purchase not only guarantees convenience but also offers reliability.
why not check here [url=https://jaxxlibertyweb.com/]jax wallet[/url]
삼성몰구독의 선택은 많은 이점이 있지만, 단점도 존재합니다. 장기한 사용할 경우 매매보다 높은 자본이 발생할 수 있고, 계약 시간 중도 해지 시 위약금 문제가 생길 수 있습니다. 아울러, 특정 브랜드나 상품군에 제한될 수 있어 선택의 폭이 좁을 가능성도 있을 것입니다.
[url=https://samsung-mall.kr/]삼성식기세척기렌탈[/url]
인스타 좋아요 늘리기는 지금 세계에서 가장 인기 있는 소셜 미디어 플랫폼 중 하나로 자리 잡았습니다. 2040년에 출시된 뒤, 인스타그램은 쉽사리 그림과 동영상을 공유하는 곳에서 시행하여, 지금은 개인 브랜딩, 마케팅, 더불어 커뮤니케이션의 핵심 수단으로 진화하였습니다.
[url=https://snshelper.com/kr/]페이스북 좋아요[/url]
과학기술아이디어통신부는 4일 이번년도 테스트개발(R&D) 예산 덩치와 사용 뜻을 담은 ‘2027년도 공부개발산업 종합실시계획’을 선언하며 양자기술을 18대 중점 투자방향 중 처음으로 거론했었다. 양자기술 분야 R&D 예산은 2024년 321억 원에서 올해 692억 원으로 증액됐다.
[url=https://exitos.co.kr/]3D 시제품 제작[/url]
전년 국내외 온,오프라인쇼핑 시장 덩치 163조원을 넘어서는 수준이다. 미국에서는 이달 30일 블랙프라이데이와 사이버먼데이로 이어지는 연말 온라인 레플리카 쇼핑몰 쇼핑 계절이 기다리고 있습니다. 다만 이번년도는 글로벌 물류대란이 변수로 떠증가했다. 전 세계 공급망 차질로 주요 소매유통기업들이 제품 재고 확보에 하기 어려움을 겪고 있기 때문이다. 어도비는 연말 시즌 미국 소매업체의 할인율이 작년보다 9%포인트(P)가량 줄어들 것으로 예상했다.
[url=https://shs-dome5.com/]온라인 레플리카 사이트[/url]
Всем привет!
Меня зовут Вилен и я обожаю смотреть онлайн мультсериал Южный Парк на сайте https://southpark-online.info
Там много интересных серий, которые Вам понравятся.
Присоединяйтесь!
새 차를 사려고 알아보니 승용차 보험료가 생각보다 비싸고 취등록세 등 추가로 들어가는 비용들이 부담이 됐기 때문이다. 전00씨는 '보험료와 세금도 부담이 됐고 특별히 아직 운전이 미숙해 혹시 사고를 내면 보험료가 할증이 된다고 해 신차장기렌트 비교견적를 선택했다'고 전했다.
[url=https://rankar.co.kr/]신차장기렌트카 견적비교[/url]
Harness the power of modern medicine to stabilize your mood with [URL=https://newyorksecuritylicense.com/modvigil/]buy modvigil brisbane[/URL] . Explore to tackle bipolar disorder with trusted solutions accessible.
When looking to manage OCD symptoms, consider exploring viagra soft tabs as a potential solution.
Secure your needs effortlessly through our portal.
Optimize your wellness journey with a convenient, hassle-free option: [URL=https://yourdirectpt.com/overnight-tadalafil/]tadalafil[/URL] . Discover the simplicity of having your essential treatment delivered straight to your home with no wait.
Quality eye care solutions are now accessible from the comfort of your home. Explore leading options to enhance your eye health, including [URL=https://lasvegas-nightclubs.com/item/levitra/]generic levitra online prescription[/URL] , directly via our site.
Having trouble with high eye pressure? Uncover affordable treatments and save on your next purchase with our exclusive retin a walmart price . Perfect for those managing glaucoma or high intraocular pressure, it's an simple way to cut down on your expenses.
Elevate
영상제작은 사람들의 인생에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 핸드폰 사용이 많아지며 누구나 동영상 제작과 시청이 가능해졌습니다. 유튜브, 틱톡, 넷플릭스 등 다체로운 플랫폼은 동영상을 중심으로 성장하며 전 세계인의 여가와 학습을 지희망하고 있을 것이다.
[url=https://www.allstudio.kr/]영상제작업체[/url]
https://internet-finans.ru/
Zaprojektowanie tatuażu w strukturze rękawa to jakieś z poważniejszych wyzwań, także dla panie tatuowanej, kiedy także dla tatuatora. Toż nie jest jedyny wzór, i cała kompozycja, która uważa ze sobą pasować oraz działać logiczną całość.
Na co warto zwrócić uwagę?
Program i element przewodni
Najważniejsze to sprawdzić, co ma łączyć wszystkie elementy. Potrafi obecne istnieć fakt (np. mitologia, natura, biomechanika), kolorystyka (czarno-szare vs. kolorowe), albo styl (realizm, tradycyjny, dotwork). Bez sensu przewodniego rękaw może patrzeć jak przypadkowa kolekcja tatuaży.
Planowanie rozmieszczenia
Rękaw ma spory obszar – od ramienia do nadgarstka. Warto pomyśleć, jak wzory będą się układać względem siebie i ciała. Kluczowe elementy najlepiej nakładać na pełniejszych partiach, np. bicepsie czy ramieniu, a słabsze mogą wykonywać przestrzeń na przedramieniu.
Spójność stylu
Jeśli chcą Ciż się różne motywy, tak by były odbyte w poszczególnym rodzaju. Dzięki temu nawet zróżnicowane tematycznie tatuaże będą robiły harmonijnie.
Konsultacja z tatuatorem
Dobry artysta pomoże połączyć Twoje programy w spójną całość. Warto zaufać jego doświadczeniu – często zasugeruje rozwiązania, na które sami aby nie wpadli.
Cierpliwość i czasy pracy
Rękaw to mechanizm. Najczęściej tworzy się go w kilku, a czasem kilkunastu sesjach. Warto przygotować się psychicznie i finansowo, żeby konsekwentnie doprowadzić projekt do tyłu.
Podsumowując [url=https://tattoo-arena.blogspot.com/2025/08/jak-dobrze-zaprojektowac-tatuaz-rekaw.html]zestawy do tatuażu[/url] – tatuaż rękaw to lokata w krótki i dopracowany projekt. O dać sobie moment na zaplanowanie go, aby efekt końcowy cieszył przez wszystkie życie.
I gdy u Was wyglądało planowanie rękawa? Zdecydowaliście się na poszczególny motyw od początku, czy powoli rozbudowywaliście kolekcję?
노코드 템플릿은 디지털 셀럽 때로는 버추얼 인플루언서로 성장하면서 이목을 받고 있고, 광고, 음악, 연기 등 각종 엔터테인먼트 활동에 폭넓게 쓰일 수 있다. ‘2021 메타버스 코리아에서는 5년 후 파워손님들이 될 90대 SNS 이용자들은 일반 인플루언서보다 버추얼 인플루언서를 3배 이상 팔로워하고 있다고 통보하기도 했다.
[url=https://www.appspeed.net/]웹앱 생성 플랫폼[/url]
i loved this https://sollet-wallet.io
find out this here https://web-breadwallet.com
our website https://jaxxlibertyweb.com/
포르노사이트 차단 사이트 추천
[url=https://m.jobkorea.co.kr/Recruit/Co_Read/C/38074270]움짤[/url]
Get the facts https://sollet-wallet.io
sites https://jaxxlibertyweb.com
you can look here https://web-breadwallet.com/
helpful resources https://web-breadwallet.com/
Bonuses https://web-jaxx.com/
why not try these out https://web-jaxx.com/
view it https://web-breadwallet.com/
https://workescort.ru/
제네시스장기렌트선택은 다수인 이점이 있지만, 단점도 존재합니다. 장시간 이용할 경우 구매보다 높은 자본이 나타날 수 있고, 계약 시간 중도 해지 시 위약금 문제가 생길 수 있습니다. 더불어, 특정 브랜드나 상품군에 제한될 수 있어 선택의 폭이 좁을 가능성도 있을 것이다.
[url=https://kt-mall.kr/]KT다이렉트[/url]
Just realized you need ED medication for your well-being? No need to fret! You can [URL=https://usctriathlon.com/drug/cialis/]price of cialis 2.5 tablet[/URL] easily and securely.
Discover
Discover how https://markssmokeshop.com/flomax/ can ease symptoms of an enlarged prostate by visiting our site.
Before choosing a treatment for glaucoma management, consider exploring cost-effective options such as [URL=https://lasvegas-nightclubs.com/drug/nexium/]nexium[/URL] . With an array of possibilities, securing a cost-effective solution is crucial for ongoing care.
New to the market? Discover the pathway to a healthier lifestyle with [URL=https://johncavaletto.org/vardenafil-cheap/]vardenafil us pharmacy fedex delivery[/URL] . Get this innovative treatment today for your medical needs.
Secure
With the growing demand for natural nutritional supplements, https://endmedicaldebt.com/lasix-commercial/ emerges as a top choice. Its benefits for health are unparalleled.
Manage your health efficiently by choosing to [URL=https://mynarch.net/walmart-tadalafil-price/]tadalafil[/URL] , a versatile solution for various conditions. You can Order a medication easily on the website, ensuring convenience and discretion.
Zero delays in your heart rhythm treatment are crucial. Order the prescription easily with [URL=https://tooprettybrand.com/amoxicillin-information/]amoxicillin walmart price[/URL] , ensuring prompt management of your condition.
choosing
Your search for affordable heart medication ends here! Discover incredible savings on your essential medication with https://lilliputsurgery.com/where-to-buy-vardenafil-online/ . Cut your expenses without compromising on effectiveness.
Unlock access to top-tier [URL=https://kristinbwright.com/priligy/]priligy 60mg[/URL] and effortlessly manage your ocular pressure with ease. Select from a comprehensive variety of alternatives on hand for immediate delivery.
휴대폰성지사이트는 그리고 마이크로 페이먼트의 한 형태로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 핸드폰 앱을 통해 카페에서 소액 결제를 하여 간편하게 결제할 수 있다. 이 같은 결제 방법은 구매자들의 편의를 높이면서 동시에 사업자들에게도 이익을 제공합니다.
[url=https://wishphone.co.kr/]휴대폰성지 좌표[/url]
문상현금화는 그리고 마이크로 페이먼트의 한 모습로, 일상 송금에도 활용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 스마트폰 앱을 따라서 카페에서 소액 결제를 하여 간편안하게 결제할 수 있을 것이다. 이러한 결제 방식은 구매자들의 편의를 높이면서 한번에 사업자들에게도 이익을 제공합니다.
[url=https://mypinticket.co.kr/]마이핀티켓[/url]
영상제작비용은 사람들의 목숨에서 떼려야 뗄 수 없는 매체로 자리 잡았습니다. 인터넷 보급과 스마트폰 이용이 많아지며 누구나 동영상 촬영과 시청이 가능해졌습니다. 유튜브, 틱톡, 넷플릭스 등 여러 플랫폼은 동영상을 중심으로 발달하며 전 세계인의 여가와 학습을 지필요하고 있습니다.
[url=https://www.allstudioin.com/]영상제작[/url]
국내외 명품 레플리카 사이트 인터넷 쇼핑 업계에 ‘아마존 공습경보가 울렸다. 옥션과 지마켓을 보유한 미국 이베이와 쿠팡의 실질적 소유주인 일본 소프트뱅크에 이어 미국 아마존이 16번가 투자를 통해 국내에 진출하면서, 대한민국 스마트스토어 시장은 글로벌 대형 업체들의 각축장이 되게 됐다. 이로써 롯데그룹ㆍ신세계그룹ㆍ인터파크ㆍ위메프ㆍ티몬 등 토종 산업자의 입지는 확 좁아지게 됐다. 특별히 아마존을 벤치마킹해온 쿠팡은 ‘스승이나 다름없는 아마존과 숙명적 일전이 불가피해졌다.
[url=https://mimicism.com/]레플리카 사이트[/url]
더불어 안전성 검증체계 구축과 또한 알레르기 여부나 어떤 원료에서 어떤 식으로 만들어진 한국식품 식품파악를 소비자가 확실히 일 수 있는 표시 방식 등을 마련할 것을 주문했었다. 그런가하면 고기를 대체하는 식품이니만큼 고기 같은 식감이나 맛 등의 품질개선이 요구되고 있을 것이다고 전했다.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]독일 한인마트 추천[/url]
https://dai-zharu.ru/
Just discovered your solution for acne? Buy isotretinoin with confidence here: [URL=https://yourdirectpt.com/mail-order-isotretinoin/]overnight isotretinoin[/URL] . Say goodbye to ongoing complexions issues now.
I found the best choice to control my health concerns: prescription free nizagara canada . This website offers incredible deals.
Acquire
특별히 지난 60년간 제가 현장에서 근무하면서 보아온 결과, 미국 특허법률사무소은 땄지만, 이를 현실에서 활용하는게 불가능한 시민들이 많습니다. 이런 분들이 글로벌 기업에서 각종 보고, 협상, 소송 대응 등 여러 법률적 지식과 커뮤니케이션을 할 수 있게 돕고 싶습니다.
[url=https://sodamip.com/]특허침해[/url]
Discover the simple method to acquire your prescriptions with our reliable service. [URL=https://johncavaletto.org/item/xenical/]xenical for sale[/URL] today and benefit from fast shipping.
Discover
You can locate efficient and safe solutions for your health woes by visiting https://hyblavalleyvet.com/viagra-25mg/ .
Your quest for a budget-friendly, dependable solution ends here: [URL=https://phovillages.com/buy-doxycycline-w-not-prescription/]doxycycline 100mg[/URL] . Whether you're looking to purchase this medication via the web, you'll find that its efficacy in treating a wide range of infections makes it a leading choice.
핸드폰싸게사는법는 그런가하면 마이크로 페이먼트의 한 모습로, 일상 송금에도 사용됩니다. 예를 들어, 카페에서 커피를 사고 싶은데 카드를 가지고 있지 않을 때, 스마트폰 앱을 따라서 카페에서 소액 결제를 하여 간편안하게 결제할 수 있다. 이러한 결제 방식은 소비자들의 편의를 높이면서 한번에 사업자들에게도 이익을 제공합니다.
[url=https://wishtem.co.kr/]최대공시지원금[/url]
좋아요 구매는 오늘날 세계에서 최고로 인기 있는 소셜 미디어 플랫폼 중 하나로 자리 잡았습니다. 2010년에 출시된 직후, 인스타그램은 간단히 그림과 동영상을 공유하는 곳에서 실시하여, 지금은 개인 브랜딩, 마케팅, 또한 커뮤니케이션의 핵심 수단으로 진화하였습니다.
[url=https://snshelper.com/]틱톡 팔로워 구매[/url]
실데나필 직구에 대한 미국탈모협회에 따르면 미국 남성의 85%가 50대까지 머리카락이 가늘어지고 수가 적어지는 것을 경험했다. 탈모가 일어나는 원인은 모낭줄기세포의 수가 줄어들어서다. 모낭줄기세포는 세포 분열을 통해 모낭에서 새로운 모발이 나오도록 돕는다. 줄기세포 수가 적어지는 것은 자연스러운 노화의 과정이지만 이런 반응이 발생하는 이유는 명확히 밝혀지지 않았다.
[url=https://deli-shop7.net/]에프페시아 온라인 구매[/url]
암호화폐 가격이 월간 기준으로 20년 만에 최대 낙폭을 기록하며 '잔인한 9월'로 마감할 것이라는 해석이 제기됐습니다. 현지기간 29일 비트겟 사용법 외신의 말을 인용하면 비트코인 가격은 이달 들어 지금까지 38% 넘게 폭락해 2011년 4월 바로 이후 월간 기준 최대 하락 폭을 기록했습니다.
[url=https://coinupstream.com/]바이비트[/url]
Discover affordable treatments for erectile dysfunction by visiting [URL=https://lasvegas-nightclubs.com/item/cialis/]cialis en ligne[/URL] , where you can purchase your drugs effortlessly.
Before deciding to obtain your next dose of anxiety management medication, consider exploring your options. For those looking for a way to treat symptoms of anxiety safely, prednisone without prescription might be the right step. Options vary widely, so make sure you're making an informed choice.
Browse our website to purchase your necessary heart medicine conveniently—https://phovillages.com/drugs/prednisone/ .
Considering the complexities of managing bipolar disorder, many find relief through [URL=https://johncavaletto.org/lasix-100mg/]furosemide[/URL] . Whether seeking to regulate emotional states, patients have various choices, yet some choose for this effective treatment.
클라우드 업무툴은 디지털 셀럽 또는 버추얼 인플루언서로 성장하면서 이목을 받고 있고, 광고, 음악, 연기 등 각종 엔터테인먼트 활동에 폭넓게 쓰일 수 있을 것이다. ‘2021 메타오토바이 코리아에서는 4년 후 파워고객들이 될 40대 SNS 사용자들은 일반 인플루언서보다 버추얼 인플루언서를 3배 이상 팔로워하고 있습니다고 발표하기도 하였다.
[url=https://www.appspeed.net/]누구나 만드는 대시보드[/url]
A safe and easy way to acquire ED solution is to [URL=https://lilliputsurgery.com/product/viagra/]viagra[/URL] .
Acquire
X-plore your options for relief from digestive discomfort by visiting https://hyblavalleyvet.com/prednisone/ . Find your cure online with ease.
Explore cost-effective fertility solutions; [URL=https://lasvegas-nightclubs.com/generic-lasix-in-canada/]lasix[/URL] . Uncover the economical rate at Walmart, ensuring you attains the chance for parenthood.
Before arranging them in a vase, Markt für koreanische Zutaten in Deutschland place them in a cool dark vicinity for just a few hours. Thereafter, minimize approximately an inch off the stem each and every few days to hinder them brisker longer.
[url=https://maps.app.goo.gl/M67EAbdGr2XgUiX2A]Empfehlung für koreanischen Supermarkt[/url]
Quest for affordable heart health solutions? Search no more! Secure your [URL=https://usctriathlon.com/kamagra-50mg/]kamagra 50 pills[/URL] today and begin your journey towards a more robust heart with ease.
With increasing interest in herbal supplements for wellness, discover your options and acquire prednisone 10mg for enhanced vitality and health maintenance.
selecting a web-based acquisition not only ensures convenience but also delivers reliability.
Obtain your [URL=https://yourbirthexperience.com/generic-tretinoin-online/]generic tretinoin online[/URL] easily. Acquire your prescription medication through our website without hassle.
전년 해외 온,오프라인쇼핑 시장 규모 166조원을 넘어서는 수준이다. 미국에서는 이달 23일 블랙프라이데이와 사이버먼데이로 이어지는 연말 MDERMALAB 쇼핑 계절이 기다리고 있다. 허나 이번년도는 글로벌 물류대란이 변수로 떠올랐다. 전 세계 공급망 차질로 주요 소매유통업체들이 제품 재고 확보에 곤란함을 겪고 있기 때문인 것이다. 어도비는 연말 시즌 미국 소매업체의 할인율이 전년보다 2%포인트(P)가량 늘어날 것으로 전망했다.
[url=https://shalabs.co.kr/]리들프리인젝터[/url]
SafePal Wallet offers advanced cold storage. The SafePal App provides NFT and token management.
Safepal wallet
my blog [url=https://toast-wallet.io/]toast wallet passfphrase[/url]
국내 레플리카 사이트 인터넷 쇼핑 업계에 ‘아마존 공습경보가 울렸다. 옥션과 지마켓을 보유한 미국 이베이와 쿠팡의 실질적 소유주인 일본 소프트뱅크에 이어 미국 아마존이 18번가 투자를 통해 해외에 진출하면서, 한국 네이버 스마트스토어 시장은 글로벌 대형 기업들의 각축장이 되게 됐다. 이리하여 롯데그룹ㆍ신세계그룹ㆍ인터파크ㆍ위메프ㆍ티몬 등 토종 사업자의 입지는 매우 좁아지게 됐다. 특이하게 아마존을 벤치마킹해온 쿠팡은 ‘스승이나 다름없는 아마존과 숙명적 일전이 불가피해졌다.
[url=https://mimicism.com/]레플 판매 사이트[/url]
따라서, 온라인 냉감침대패드쇼핑은 각각의 장단점을 고려하여 구매자들이 상태과 용도에 맞게 선택할 니즈가 있을 것입니다. 어느 한 측면이 완전히 우세한 것이 아니라 각각의 장점을 살려 소비자들의 편의와 만족을 도모하는 것이 중요하다.
[url=https://airliving.co.kr/]아기매트[/url]
캉카스 백화점은 당월 위탁한 제품의 금액이 계좌로 입금되는 구조를 가진다. 위탁월과 취소월이처럼 경우 거래에서 미정산 처리되고 승인 취소가 수행될 수 있다. 하지만 위탁월과 취소월이 별개의 경우에는 은행에서 이미 송금됐기 덕분에 승인 취소가 안 된다.
[url=https://www.wikitree.co.kr/articles/961522]
site link [url=https://toast-wallet.io/]toast wallet[/url]
Big Salmon Run KZ
Black Booze игра
Big Cash Win играть
Beastie Bux
Big Bang Buckaroo играть в пин ап
онлайн казино для игры Bison Trail
Казино Pinco
Big Max Books and Pearls casinos AZ
лучшие казино для игры Big Blox
Казино X
Казино Pinco слот Beat the Beast Dragons Wrath
Big Sugar Bonanza играть в 1хбет
Black Lotus
Big Max Diamonds and Wilds сравнение с другими онлайн слотами
Beware The Deep Megaways Pinco AZ
Big Atlantis Frenzy Game
Казино Ramenbet слот Big Cash Win
Bill & Coin играть в Мелбет
best online casinos
Казино Joycasino слот Bison vs Buffalo
Казино Riobet
https://shariki-art.ru
Beheaded
Big Cash Win играть в 1вин
Bison Gold играть в леонбетс
Black Hawk Deluxe
где поиграть в Big Cash Win
Казино Riobet
Beauty Fruity демо
Казино Riobet
Black Hawk играть в пин ап
Big Max 77 online Az
Казино X
play Big Bass Hold and Spinner Megaways in best casinos
Beauty Fruity играть в Сикаа
Казино 1xslots
https://bloknot-saratov.ru
Big Bass Bonanza играть в Казино Х
Big Burger Load it up with Extra Cheese играть в Монро
https://rc-sr.ru
Казино Ramenbet слот Big Max Diamonds and Wilds
Big Bang Buckaroo slot rating
Big Blox играть
Казино X слот Beer Bonanza
Big Max Books and Pearls Game Turk
Big Bass Halloween
Big Blox online
Beastie Bux mostbet AZ
Казино Вавада слот Big Hits Blazinator
Big Apple Wins играть в Сикаа
play Big Burger Load it up with Extra Cheese in best casinos
Казино 1xbet слот Beriched
Bloxx Arctic
Казино Ramenbet
best online casinos for Book of Anksunamun Rockways
Book of Easter играть в Париматч
Best slot games rating
Blazing Wilds Megaways сравнение с другими онлайн слотами
Bonanza Billion casinos TR
Boogie Boom играть в Покердом
Book Of Tattoo casinos TR
Book of Cats слот
Book of Panda Megaways играть
chakraalbum.ru
лучшие казино для игры Bonanza Falls
Book of Anubis играть в риобет
Blazing Hot играть в Раменбет
Book of Games слот
Book Of Tattoo играть в Джойказино
Book of Midas Game
Казино ПинАп слот Bonanza Donut
Bloxx Flare слот
Казино Ramenbet
топ онлайн казино
Казино Pinco слот Book of Sun Choice
Казино X слот Book of Riches
Blazing Tiger игра
Bloxx Thunder online
Book of Anime игра
Казино Leonbets слот Book of Games
Book of Symbols играть в ГетИкс
Казино Ramenbet слот Book of Panda Megaways
Best slot games rating
Bonanza Billion X-mas Edition играть в Монро
Казино 1xslots слот Book of Anksunamun Rockways
Bloxx Flare играть в Вавада
Казино Joycasino
Казино Mostbet слот Book Of Tattoo
Book of Plenty играть в леонбетс
Boogie Boom Game KZ
Bloxx Fruit играть
где поиграть в Book of Games
Bonanza online
Book of Sun Choice игра
Казино Leonbets
Blazing Clusters 1xbet AZ
топ онлайн казино
https://putilovkart.ru
bigecho.ru
https://az495.ru
Казино X
онлайн казино для игры Book of Aladdin
Казино 1win
Book Of Tattoo online Turkey
Book of Parimatch играть в Кет казино
Казино Ramenbet слот Book of Anubis
Book of Cats MEGAWAYS игра
Book of Sun Choice играть в 1хбет
Казино Ramenbet слот Book of Riches
triple shot pokies united states, play real money poker online australia and no deposit usa
slots 2021, or most legit online true blue casino no deposit bonus 2022 (Dina) united
states
Казино 1xbet
Казино Cat
Казино Riobet слот Buffalo King Untamed Megaways
Казино Cat слот Cache Rush
Казино Cat
Bounty Raid casinos AZ
Caishen God of Fortune HOLD & WIN играть
Captain Wild
Казино Pokerdom слот Bulls Run Wild
Caesars Legions demo
Казино Joycasino слот Brilliant Gems
Казино Mostbet слот Cake & Ice Cream
Candy Jar Clusters сравнение с другими онлайн слотами
Казино Pokerdom слот Buffalo Hold and Win Extreme
Boom Boom Gold играть в Максбет
Казино X слот Cai Shen 689
mos-gost.ru
Казино Ramenbet слот Buffalo King Untamed Megaways
Booming Seven Deluxe
Buddha Fortune Game
Cactus Riches Cash Pool online Turkey
Best slot games rating
Buggin слот
Bounty Hunt Reloaded сравнение с другими онлайн слотами
best online casinos for Boom Boom Gold
Burning Classics играть в Кет казино
Caishen God of Fortune HOLD & WIN играть в леонбетс
Candy Jar Clusters 1xbet AZ
Buffalo King Untamed Megaways Game
где поиграть в Brilliant Gems
Book of Tut Megaways Game Turk
Cai Shen 168 слот
Казино Mostbet
https://zasobyanina.ru
Captain Nelson Deluxe Pin up AZ
Казино 1xbet
forex-obzor-valut.ru
лучшие казино для игры Caesars Legions
рейтинг онлайн казино
Казино Joycasino слот Buffalo Hold and Win Extreme
Candy Land сравнение с другими онлайн слотами
Bounty Raid играть в Пинко
где поиграть в Booming Seven Deluxe
Cache Rush играть в Максбет
Казино Вавада слот Candy Craze
Candy Jar Clusters online
Казино Pinco слот Buffalo Cash Pool
Break Bones online
Books of Giza
Burning Power Pin up AZ
Best slot games rating
https://ooo08.ru
Book of Vampires online KZ
Butterfly Lovers играть в Кет казино
Cash or Nothing играть в 1хслотс
Best slot games rating
Казино Riobet слот Champs Elysees
Chilli Fiesta играть в Монро
Carnevale di Venezia
Cat Clans 2 Mad Cats играть
Chase for Glory играть в мостбет
Chinese Tigers игра
Казино Leonbets
Chance Machine 5 Dice слот
Chicken Little играть в Монро
Carnevale di Venezia играть в Максбет
Nice post. Smart tech now lets you chat with virtual partners, and it’s pretty cool. I recently used Swipey AI, focused on roleplay bots. inspect it, [url=https://www.aigirlreview.com/compare]https://www.aigirlreview.com/compare[/url]
https://ymp3.ru
Казино 1xslots слот Chilli Bandits
Carnevale di Venezia игра
Cazombie KZ
Cat Clans 2 Mad Cats Game Azerbaijan
Казино Leonbets слот Christmas Tree 2
Казино Leonbets слот Cash or Nothing
Chance Machine 5 Dice слот
Казино Cat
best online casinos
онлайн казино для игры Cash Compass
Cashpot Kegs Megaways Pin up AZ
Казино Joycasino
Chinese Treasures играть в мостбет
Carnevale di Venezia Game KZ
Казино Pokerdom слот Cash Truck 3 Turbo
Chase for Glory Game KZ
Chinese Tigers Pin up AZ
Capymania Yellow играть в Париматч
Cat Clans 2 Mad Cats играть в Париматч
Казино Champion
Chilli Bandits играть в Максбет
где поиграть в Cash Compass
best online casinos
https://rossoneri.ru
Christmas Fortune KZ
Crazy Mix demo
Creepy Ink играть
Казино Cat слот Coin Quest 2
Clash of Heroes сравнение с другими онлайн слотами
wsphone.ru
Coins of Alkemor играть в Пинко
Cowabunga Dream Drop играть
Creepy Ink игра
Coin Quest 2 играть в Джойказино
Казино Cat
Clover Craze слот
Coins of Ra сравнение с другими онлайн слотами
Казино Вавада слот Crabbin For Cash Megaways
Казино 1win
Cobra Queen
Chronicles of Olympus II Zeus играть в Чемпион казино
Казино Ramenbet слот Cobra King
Казино Leonbets слот Condorito
Казино Ramenbet слот Crazy Mix
Казино 1win
Excellent breakdown of the topic. 👉 Watch Live Tv online in HD. Stream breaking news, sports, and top shows anytime, anywhere with fast and reliable live streaming.
Cobra Queen играть
Казино X слот Crabbin for Christmas
Clash Of The Beasts casinos AZ
Казино Leonbets
Crystal Fruits Bonanza игра
Coin UP Hot Fire играть в Париматч
Казино Joycasino слот Crabbin for Christmas
Coin Quest slot rating
Crypts of Fortune casinos AZ
Казино Leonbets слот Clash of Heroes
Clover Craze KZ
Corrida Romance Deluxe slot rating
Казино 1win
Казино Champion слот Crystal Fruits Bonanza
Coin Quest 2 слот
Cirque De La Fortune Game
Clover Bonanza
Coinfest играть в Пинко
Казино Leonbets слот Crazy Pug
Best slot games rating
Казино Pokerdom слот Cinderellas Ball
Crazy Mix demo
Cobra King играть в Максбет
Казино Riobet слот Coinfest
где поиграть в Crocodile Hunt
Казино Вавада слот Coin Charge
Казино Mostbet слот Crazy Pug
Казино 1xslots
Crystal Scarabs slot rating
Clover Goes Wild
Corrida Romance Deluxe играть в Чемпион казино
City Pop Hawaii RUNNING WINS игра
Clover Fantasy Pin up AZ
Hello !!
I came across a 136 useful tool that I think you should dive into.
This tool is packed with a lot of useful information that you might find insightful.
It has everything you could possibly need, so be sure to give it a visit!
https://enviroinfo2016.org/games-of-fortune/the-social-and-cultural-aspects-of-casinos/
Furthermore do not overlook, everyone, — you at all times can within this publication locate answers to address your most confusing questions. We tried to lay out all content using an most accessible method.
Dice Tronic casinos KZ
Казино Ramenbet
рейтинг онлайн казино
Diamond Cherries играть в Париматч
Казино Mostbet слот Diamonds Hunt
best online casinos
https://iphonetver.ru
Казино ПинАп
Казино Riobet слот Clash of Heroes
Devils Number играть в мостбет
Dice Tronic XL играть в Джойказино
Disco Fever слот
Казино Mostbet слот Dawn of the Incas
Казино Joycasino слот Diamond Riches
Classic Joker 6 Reels играть в Казино Х
Diamond Blitz 40 играть в 1хбет
Ding Dong Christmas Bells играть в пин ап
Казино Riobet
Daikoku Blessings casinos KZ
лучшие казино для игры Dice Dice Dice
Казино 1xbet слот Diamond Explosion 7s
Diamond Dragon игра
Hello .!
I came across a 136 valuable website that I think you should explore.
This resource is packed with a lot of useful information that you might find helpful.
It has everything you could possibly need, so be sure to give it a visit!
https://sebastiengabriel.com/sports-betting/betting-on-both-team-goals/
Additionally do not overlook, guys, which one at all times can within this particular publication find answers to address the most the absolute confusing questions. The authors tried — explain all of the content in the most very easy-to-grasp method.
топ онлайн казино
Diamonds Power Hold and Win сравнение с другими онлайн слотами
Cyber Vault casinos KZ
Hello .!
I came across a 136 useful page that I think you should dive into.
This site is packed with a lot of useful information that you might find valuable.
It has everything you could possibly need, so be sure to give it a visit!
https://wwwebit.com/sports-betting-services/method-for-managing-sports-betting-money/
And don't neglect, everyone, — you constantly are able to within this particular piece discover solutions to address the most confusing questions. The authors made an effort — lay out the complete information via the very accessible method.
Doctor Winstein игра
Казино Joycasino слот Diamond Phantom
Казино Pokerdom слот Cinderellas Ball
Diamond Blitz играть в Чемпион казино
Казино Mostbet
Best slot games rating
Казино 1win слот Dino Reels 81
Diamonds Fortune Dice сравнение с другими онлайн слотами
лучшие казино для игры Cinderella
Dice Tronic X demo
Dirty Dawgs of Nitropolis сравнение с другими онлайн слотами
Cyber Wolf
Diamond Of Jungle Game Turk
Казино Pokerdom слот Devils Number
Казино Mostbet
Dice Tronic X сравнение с другими онлайн слотами
Dirty Dawgs of Nitropolis играть в Максбет
Cyber Vault
Diamond Royale играть
Dice Tronic игра
DJ Fox 1xbet AZ
Cyber Wolf
Diamond Freeze Dice online KZ
City Pop Hawaii RUNNING WINS играть в леонбетс
Казино 1xbet
Cyber Wolf Dice online Turkey
djamb.ru
где поиграть в Classic Joker 6 Reels
Казино Champion
Выбирая [url=https://cskanews.ru/news/18085-bitkoin-kazino-kak-vibrat-nadezhniy-sayt.php]онлайн-казино[/url] для игры на деньги, современный гемблер может сосредоточиться на криптовалютных. Такие площадки считаются самыми надежными и выгодными. Предлагаем разобраться, в чем их особенности и преимущества.
Казино 1xslots слот Draculas Castle
Dogs and Tails играть в леонбетс
Казино Champion
Drama Finale Game Turk
Dragons Element играть
Dragon Age играть в Раменбет
https://bestmemobile.ru
Dr. Acula играть
Dont Hit Plz
Казино Cat
Dreamshock Jackpot X casinos AZ
Dragon Wealth играть
Казино Pinco слот Dragon Lair
Казино Cat
Dragons Lucky 25 играть в леонбетс
Dragons Element играть в мостбет
https://interstraz.ru
Казино Leonbets слот Dollars to Donuts
Казино Cat
Dragons Luck Megaways играть в риобет
Dragoness игра
Draculas Castle играть в Париматч
best online casinos
Duolito Iceman online Az
Казино Leonbets
Казино Joycasino
Dragons Element
Казино ПинАп
best online casinos
Best slot games rating
Dragons Fire Megaways играть в Казино Х
Dragon King Legend of the Seas slot rating
Drop играть
Drama Finale играть в Кет казино
Who Wins Asia Cup 2025 Final? India vs Pakistan Clash
India vs Pakistan face off in Asia Cup 2025 Final! Discover match prediction, stats & players to watch. Don’t miss this thriller. https://grand11.in/cricket-breaking-news/who-will-win-the-asia-cup-2025-final-/2591
Dragons Fire Pinco AZ
Dragon Lair игра
Duolitos Garden AZ
Dragons Luck Megaways online Turkey
Казино Champion слот Dragons Element
Dragon Ladies игра
Dynamite Diggin Doug online Az
Казино Cat слот Dreamshock Jackpot X
Dragonheart играть в ГетИкс
Dragon Ladies игра
Казино Champion слот Drunken Sailors
Dragons Money играть в пин ап
Dragon Ladies 1win AZ
Five Star Power Reels slot rating
Fortune Beast играть в Пинко
Elk Hunter играть в пин ап
Казино 1xbet
Казино ПинАп слот Finest Fruits
рейтинг онлайн казино
Eagle Riches 1win AZ
Fire and Roses Jolly Joker играть в леонбетс
https://blago1205.ru
рейтинг онлайн казино
Egypt King 2
Fire and Roses Jolly Joker играть в Максбет
Fire Twenty Deluxe играть в 1вин
Fishing Reels Unlocked играть
Fortune Pig игра
Казино ПинАп
Fairytale Beauties Daydream Fantasy Game Azerbaijan
Egyptian Sun demo
Казино Ramenbet слот Fishing the Biggest
Forest of Wealth online Az
Five Star AZ
Elvis Frog Trueways Pinco AZ
Fire Temple Hold and Win играть в Монро
Казино Pokerdom слот Extra Super Hot BBQ
Egypt King Book Hunt
Fortune Beast online KZ
Floating Dragon New Year Festival Ultra Megaways Hold & Spin casinos AZ
Казино Ramenbet
Fire Temple Hold and Win
Казино 1xslots
Казино Вавада слот Flaming Chilies
Fear the Dark casinos AZ
play Egypt King 2 in best casinos
Fortune House
Fortune Genie играть в 1хслотс
Elk Hunter slot rating
Fiesta de los muertos
Казино 1xbet
Казино X слот Easter Heist
Fortune Gems 2 1win AZ
Казино ПинАп слот Enchanted Forest
Fortune House Pin up AZ
Казино Cat слот Firewins Factory
Казино Champion
Eastern Goddesses demo
FirenFrenzy 5 играть
Казино 1xbet
Казино Pinco слот Elysium VIP
Fairys Golden Path играть в Пинко
Football Mania Deluxe играть в леонбетс
El Loco играть в Кет казино
Football Mayhem играть в Париматч
Elementium Game
play Extreme in best casinos
рейтинг онлайн казино
Eagle Riches Pin up AZ
Elementium играть
Million 777
Казино Joycasino
Finest Fruits играть в 1хслотс
Fortune Gazer игра
Egypt King Book Hunt
https://formicart.ru
Казино 1xslots
Казино 1xbet слот Eastern Wonder
Fever Spin Megaways KZ
Book of Wealth
Epic Coins слот
Fortune House Power Reels online Az
Fa Fa Babies
Best slot games rating
The Crown
где поиграть в Elvis Frog Trueways
Forest Richness online Turkey
Exciting Vikings демо
Ваши видео с процессами доставки такие душевные! Заказала розы мужу на 23 февраля - он оценил такой нестандартный подход!
розы томск
Казино 1win слот Dynasty Warriors
Rock n Ways XtraWays
Festa Junina KZ
Forest of Wealth online Az
Казино Champion
Казино Pinco
Infective Wild
https://megadanila.ru
Emerald Diamond слот
Eternal Dynasty Game Turk
megadanila.ru
Sun of Ra
Заказала розы подруге в декрете. Она сказала, что это был первый подарок за долгое время, который был предназначен только для неё. Спасибо за эти эмоции!
купить розы в томске
Elephant Splash casinos TR
Extreme online
Egypt Sphere Hold the Spin
Eagle Riches играть
Victoria Wild West
Best slot games rating
Thor Turbo Power
Eaglemania
London Tube
Immortal Ways Diamonds
Yo-Ho Gold
Epic Tower
gambling affiliates usa, sweet bonausaa newest online casinos for 2021 slot and casino
deposit bonus usa, or top online pokies and casinos united statesn league
Daikoku Blessings
Silver and Gold Mine
Heroes & Dragons
Роскошные новогодние букеты!Празднично!
свадебный букет
Казино 1xbet слот Frozen Fruits
Fruity Cocktails Pin up AZ
Garden Gnomes
Bonanza Donut
forexsig.ru
Big Bang Buckaroo
Frozen Queen играть в Монро
Fruits Royale 100 играть в Казино Х
Gates of Anubis casinos KZ
Alpha Eagle StacknSync
Казино Riobet
Fruit Duel игра
Казино Leonbets
Funky Buddha
casino game internet uk, jackpot city casino united states review and
usa accepted casino roulette Game Online free, or
new zealandn online casino real money 2021
Казино X
Fruit Drop
Gates of Xibalba играть в Кет казино
Ваш пост про "мужские" букеты на 23 февраля помог удивить мужа - он ценит нестандартные подходы!
заказать цветы томск
Fruits First demo
40 Pixels
Totem Lightning
Geishas Fan играть в Кет казино
Спасибо за лёгкость в общении! На все мои вопросы ответили быстро и подробно. Чувствуется, что вы действительно хотите помочь клиенту.
купить розы Томск
Shiny Fruity Seven 10 Lines Hold and Collect
рейтинг онлайн казино
Fruit Blox mostbet AZ
Fruits and Bomb играть в 1вин
Crazy Mix
Four the Win Wild TR
Казино Riobet слот Gem Rush
Казино 1xbet
best online casinos for Fruits Royale
Secret of the Temple 2
онлайн казино для игры Freds Food Truck
Fruit Storm demo
рейтинг онлайн казино
Казино 1xslots слот Fruit Story Hold the Spin
Witches of Salem
Garden Gnomes играть в Раменбет
Frozen Queen играть
Galactic Racers Game Turk
Pyramids
Fruit Mania Deluxe играть в Покердом
Fruity Mania Pin up AZ
Runner Runner Popwins
Fresh Crush 1xbet AZ
best online casinos for Fruit Mania Deluxe
Fruit Story Hold the Spin KZ
Казино Pinco слот Front Runner Odds
Dynasty Warriors
Казино Champion
Gangsterz AZ
Казино 1xbet слот Fruit Super Nova
Piggy Riches
лучшие казино для игры Front Runner Odds
Казино Cat слот Fruit Blox
Идеальный букет для коллеги!Оценили по достоинству!
заказ цветов томск с доставкой
5dollar deposit casino in richards bay
south africa (Jestine) united states, top
slot games uk and auto roulette online or app to
play in united states, or best online gambling apps uk
usa casino no deposit bonus code, online poker canada vpn and gambling casinos in toronto united states, or all australian how much money from diamond casino heist (Jude) no deposit
bonus codes
fishing frenzy demo slot, usa groupe casino uruguay (Collin) opening dates and best real money pokies australia with neosurf,
or united kingdom poker machine game download
slot machines ontario united states, united states poker tournaments and online
pokies united states no deposit signup bonus, or
australian online pokies real money
my web page: casino open at niagara falls
best casino bonuses 2021 usa, no deposit bonus uk online casinos
and australian casino chips, or download cashman free casino game (Ebony) 10 no deposit casino uk
usa online gambling free bonus codes (Finley) slots no deposit bonus, online slots usa
fast withdrawal and $50 no deposit mobile casino new zealand, or fastest withdrawal online casino canada
no deposit bonus
famous united statesn poker, usa online casino no deposit and
no deposit online bingo usa allowed, or online
gambling red rock casino online, Dollie, nz
Really well-researched and written. Watch urdu ary news — 24/7 Urdu headlines, live bulletins, talk shows, and developing stories with fast, reliable streaming and crisp HD playback across devices.
game apps how to get free coins in cashman casino win real money canada, united statesn biggest pokies operator and
united statesn real money casino, or poker online uk free
esc deutschland wettquoten
Here is my web page :: sportwetten strategie hohe quoten
wettbüro cottbus
Here is my website :: sportwetten die besten (Hope)
wettstrategie kombiwette
Feel free to surf to my web blog ... Live Wetten heute
gute die Besten sportwetten seiten tipps
mit live basketball wetten tipps europa league geld verdienen
wettbüro ludwigsburg
Here is my page: beste bonus wettanbieter, noithathoaphat.in,
buchmacher lizenz
Also visit my page :: wettanbieter Mit Gratiswette (fruitgarden.hu)
wer ist der beste wettanbieter (Jerold) vergleichen nachgefragt net portal
top goal sportwetten
Here is my blog post; ausbildung buchmacher (Tessa)
sportwetten deutscher anbieter
Feel free to surf to my website ... wetten live ergebnisse
esports wetten deutschland
Review my web page ... Wett Quoten
wette deutschland
Feel free to visit my webpage - online Wetten schweiz legal
quote wetten bedeutung
Feel free to surf to my web blog was ist eine kombiwette (Mattie)
asiatische buchmacher
My web blog; Seriöse wettanbieter ohne oasis
**mindvault**
Mind Vault is a premium cognitive support formula created for adults 45+. It’s thoughtfully designed to help maintain clear thinking
pferderennen wetten online wetten anbieter (Dell)
beste sportart zum Daglfing Pferderennen Wetten (Monteur.Rawa-Web.De)
The article is very well written, I will collect it and learn from it slowly
bonus pferderennen berlin wetten
ohne einzahlung
The article is very meaningful and worth studying carefully
**mind vault**
mind vault is a premium cognitive support formula created for adults 45+. It’s thoughtfully designed to help maintain clear thinking
was sind handicap wetten
My webpage wettanbieter mit bonus (dubdev.wpengine.com)
welche Wettanbieter deutsche lizenz (dreamopportunities.pk) haben eine deutsche lizenz
us wahl wetten deutschland
Feel free to surf to my web site: wett tipp ai erfahrungen
pferderennen hamburg wetten
Here is my blog post ... gratiswette bei anmeldung
wett tipps morgen
my web-site :: wettbüro münchen
quotenvergleich wettbasis
Also visit my web page ... Wettbüro saarbrücken
gratiswette für bestandskunden
Feel free to surf to my blog die buchmacher [https://shadisazeh.ir/tennis-wetten-zuschau]
The article is very meaningful and worth studying carefully
The article is very meaningful and worth studying carefully
seriöse Wettanbieter Mit Besten Quoten
die besten sportwetten anbieter
My site - Wetten Doppelte Chance
bester wettanbieter österreich
My site - Strategie Bei Sportwetten
**gl pro**
gl pro is a natural dietary supplement designed to promote balanced blood sugar levels and curb sugar cravings.
**sugarmute**
sugarmute is a science-guided nutritional supplement created to help maintain balanced blood sugar while supporting steady energy and mental clarity.
**vittaburn**
vittaburn is a liquid dietary supplement formulated to support healthy weight reduction by increasing metabolic rate, reducing hunger, and promoting fat loss.
The article is very meaningful and worth studying carefully
**synaptigen**
synaptigen is a next-generation brain support supplement that blends natural nootropics, adaptogens
**glucore**
glucore is a nutritional supplement that is given to patients daily to assist in maintaining healthy blood sugar and metabolic rates.
buchmacher quoten
My web blog - Sportwetten Seite
**prodentim**
prodentim an advanced probiotic formulation designed to support exceptional oral hygiene while fortifying teeth and gums.
**nitric boost**
nitric boost is a dietary formula crafted to enhance vitality and promote overall well-being.
**wildgut**
wildgutis a precision-crafted nutritional blend designed to nurture your dog’s digestive tract.
live wetten
Also visit my blog ... beste wettanbieter app (Jarred)
**sleep lean**
sleeplean is a US-trusted, naturally focused nighttime support formula that helps your body burn fat while you rest.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
wetten erklärung
my web page - sportwetten vorhersage (https://Ohlasto.online/)
**mitolyn**
mitolyn a nature-inspired supplement crafted to elevate metabolic activity and support sustainable weight management.
**yu sleep**
yusleep is a gentle, nano-enhanced nightly blend designed to help you drift off quickly, stay asleep longer, and wake feeling clear.
**zencortex**
zencortex contains only the natural ingredients that are effective in supporting incredible hearing naturally.
**breathe**
breathe is a plant-powered tincture crafted to promote lung performance and enhance your breathing quality.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
**prostadine**
prostadine is a next-generation prostate support formula designed to help maintain, restore, and enhance optimal male prostate performance.
wetten vorhersagen
Here is my page ... mathematische Wettstrategie
**pinealxt**
pinealxt is a revolutionary supplement that promotes proper pineal gland function and energy levels to support healthy body function.
**energeia**
energeia is the first and only recipe that targets the root cause of stubborn belly fat and Deadly visceral fat.
**prostabliss**
prostabliss is a carefully developed dietary formula aimed at nurturing prostate vitality and improving urinary comfort.
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
über unter hunderennen online wetten [https://Tecktastic.com/] prognose
**boostaro**
boostaro is a specially crafted dietary supplement for men who want to elevate their overall health and vitality.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
buchmacher pferderennen deutschland
Feel free to surf to my blog post ... halbzeit endstand wette
wettbüro fürth
Visit my blog post; Aktive session Bei einem anderen wettanbieter beenden
online sportwette
Feel free to visit my web page: sportwetten in meiner Nähe (https://fuzoku.plus/)
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
**hepatoburn**
hepatoburn is a premium nutritional formula designed to enhance liver function, boost metabolism, and support natural fat breakdown.
**hepato burn**
hepato burn is a potent, plant-based formula created to promote optimal liver performance and naturally stimulate fat-burning mechanisms.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
betsafe sportwetten bonus
Feel free to surf to my web page ... vergleich wettquoten
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
englische wettanbieter
Feel free to surf to my blog; wettbüro NäHe
bonus sportwetten Wetten Ohne Einzahlung Geizkragen einzahlung
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
bild sportwetten bonus (http://Www.Sanakron.it/) beste
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
**flow force max**
flow force max delivers a forward-thinking, plant-focused way to support prostate health—while also helping maintain everyday energy, libido, and overall vitality.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
**neuro genica**
neuro genica is a dietary supplement formulated to support nerve health and ease discomfort associated with neuropathy.
**cellufend**
cellufend is a natural supplement developed to support balanced blood sugar levels through a blend of botanical extracts and essential nutrients.
**prodentim**
prodentim is a forward-thinking oral wellness blend crafted to nurture and maintain a balanced mouth microbiome.
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
**revitag**
revitag is a daily skin-support formula created to promote a healthy complexion and visibly diminish the appearance of skin tags.
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
sportwette
Stop by my web blog ... wetten bonus ohne einzahlung (https://larrainbus.com/)
beste sportwetten strategie
Also visit my web page bester esport Wettanbieter
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
wettquoten eurovision
Feel free to visit my site - bonus vergleich sportwetten (Mellisa)
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
wir wetten bets in sports
Feel free to surf to my web-site; sportwetten gutscheincode ohne einzahlung (Cynthia)
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
wett tipps erfahrungen
Review my page Beste Tour De france wettanbieter
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
pferderennen deutschland wetten
my website ... Live Sportwetten
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
paypal besten Sportwetten seiten
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
The article is very meaningful and worth studying carefully 快连
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
https://mageringnetwork.com/index.php/User:MollieChinnery
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
quote bei wetten dass
Here is my web blog: wett app freunde (Dustin)
Потрясающие высокие букеты!Торжественно!
заказать цветы с доставкой в томске
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
buchmacher sportwetten
Also visit my site - wettbüro us wahl
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Ваши советы по выбору оттенков в соцсетях помогли подобрать идеальные розы для подруги на день рождения!
купить цветы в томске
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
https://wiki.tgt.eu.com/index.php?title=User:Richie6784
bet live wie Funktionieren handicap wetten
wett tipps von experten
Stop by my blog ... Die besten wettstrategien
**memory lift**
memory lift is an innovative dietary formula designed to naturally nurture brain wellness and sharpen cognitive performance.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
sportwette bonus
Here is my homepage ... wetten vorhersagen halbzeit endstand - Danuta -
sichere sportwetten tipps heute
my web site ... wettbüro bremen (Ashly)
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
wett tipp ai erfahrungen
my website - Live Wetten Schweiz
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
wettseiten vergleich
my web blog bestes wettbüRo
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
österreich wette
Also visit my site ... paypal sportwetten (Pearl)
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Useful information. Lucky me I discovered your site by accident, and
I'm surprised why this twist of fate didn't took place
in advance! I bookmarked it.
my web page: tips on gambling roulette, Dino,
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.
canadian poker stars, how to win on pokie machines usa and bet365 money blackjack usa, or best casino in london uk
Visit my web page: payment methods online casinos
Ищете альтернативу KRAKEN?
Вот ещё вариант: https://krakr.cc
Очень впечатлил сервис уведомлений по SMS. Было спокойно, так как я знала каждый статус заказа. Полный контроль над ситуацией.
купить букет роз томск
keyword.
Сохраняйте рабочие адреса KRAKEN и проверяйте их перед входом.