To gauge hospital quality, patients deserve more outcome measures
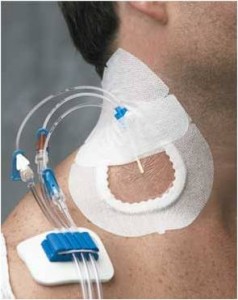 Patients, providers and the public have much to celebrate. This week, the Centers for Medicare and Medicaid Services’ Hospital Compare website added central line-associated bloodstream infections in intensive care units to its list of publicly reported quality of care measures for individual hospitals.
Patients, providers and the public have much to celebrate. This week, the Centers for Medicare and Medicaid Services’ Hospital Compare website added central line-associated bloodstream infections in intensive care units to its list of publicly reported quality of care measures for individual hospitals.
Why is this so important? There is universal support for the idea that the U.S. health care system should pay for value rather than volume, for the results we achieve rather than efforts we make. Health care needs outcome measures for the thousands of procedures and diagnoses that patients encounter. Yet we have few such measures and instead must gauge quality by looking to other public data, such as process of care measures (whether patients received therapies shown to improve outcomes) and results of patient surveys rating their hospital experiences.
Unfortunately, we lack a national approach to producing the large number of valid, reliable outcome measures that patients deserve. This is no easy task. Developing these measures is challenging and requires investments that haven’t yet been made.
Read More »To gauge hospital quality, patients deserve more outcome measures
 I was reminded again recently of how important it is to sometimes just sit back and listen to what our patients have to say. Every month, as part of our hospital-wide patient safety efforts, I meet with staff and interview patients, seeking to learn how we can improve the care we provide to them.
I was reminded again recently of how important it is to sometimes just sit back and listen to what our patients have to say. Every month, as part of our hospital-wide patient safety efforts, I meet with staff and interview patients, seeking to learn how we can improve the care we provide to them. Far too many patients are harmed rather than helped from their interactions with the health care system. While reducing this harm has proven to be devilishly difficult, we have found that checklists help. Checklists help to reduce ambiguity about what to do, to prioritize what is most important, and to clarify the behaviors that are most helpful.
Far too many patients are harmed rather than helped from their interactions with the health care system. While reducing this harm has proven to be devilishly difficult, we have found that checklists help. Checklists help to reduce ambiguity about what to do, to prioritize what is most important, and to clarify the behaviors that are most helpful.
 Last year, Sarah Andryauskas, then a new nurse in our emergency department, was caring for a patient with diabetes who had trouble maintaining healthy blood glucose levels. His disease had contributed to several hospital visits over the preceding months and years.
Last year, Sarah Andryauskas, then a new nurse in our emergency department, was caring for a patient with diabetes who had trouble maintaining healthy blood glucose levels. His disease had contributed to several hospital visits over the preceding months and years. I recently gave a talk to the American Medical Student Association. The energy in the room was palpable. The students were excited, passionate and hopeful. We spoke about the urgent need to reduce preventable harm and to enhance value, and we discussed that they will need to be the ones to lead these efforts.
I recently gave a talk to the American Medical Student Association. The energy in the room was palpable. The students were excited, passionate and hopeful. We spoke about the urgent need to reduce preventable harm and to enhance value, and we discussed that they will need to be the ones to lead these efforts.